‘In process ~ 3-4 April 2025.’
C19.Life (4 Apr 2025)
‘50 papers on the brain and nervous system.’
Source (Date)
📖
(1 Aug 2024 ~ University of Oxford)
‘Long-term cognitive and psychiatric effects of COVID-19 revealed in new study’.
➤
‘first wave unvaxxed’
© 2024
University of Oxford.
📖
(31 Jul 2024 ~ The Lancet: Psychiatry)
‘Cognitive and psychiatric symptom trajectories 2–3 years after hospital admission for COVID-19: a longitudinal, prospective cohort study in the UK’.
➤
‘xxx’
© 2024
Taquet
et al
/
The Lancet: Psychiatry.
📖
(25 Jan 2024 ~ The Lancet: eClinicalMedicine)
‘Long COVID is associated with severe cognitive slowing: a multicentre cross-sectional study’.
➤
‘xxx’
© 2024
Zhao
et al
/
The Lancet: eClinicalMedicine.
📖
(30 Jan 2025 ~ Nature: Medicine)
‘Plasma proteomic evidence for increased β-amyloid pathology after SARS-CoV-2 infection’.
➤
‘xxx’
© 2025
Duff
et al
/
Nature: Medicine.
📖
(7 Mar 2022 ~ Nature)
‘SARS-CoV-2 is associated with changes in brain structure in UK Biobank’.
➤
‘xxx’
© 2022
Douaud
et al
/ Nature.
📖
(17 Aug 2024 ~ Nature: Scientific Reports)
‘Patients recovering from COVID-19 who presented with anosmia during their acute episode have behavioral, functional, and structural brain alterations’.
➤
‘xxx’
© 2024
Kausel
et al
/
Nature: Scientific Reports.
📖
(21 Jul 2023 ~ The Lancet: eClinicalMedicine)
‘The effects of COVID-19 on cognitive performance in a community-based cohort: a COVID symptom study biobank prospective cohort study’.
➲
‘xxx’
© 2023
Cheetham
et al
/
The Lancet: eClinicalMedicine.
📖
(10 Nov 2023 ~ Journal of the American Geriatrics Society)
‘Post-acute sequelae of SARS-CoV-2 (PASC) in nursing home residents: A retrospective cohort study’.
➤
‘Nursing Home residents experienced a significant functional decline that persisted for 9 months following acute infection.’
© 2023
Clark
et al
/
Journal of the American Geriatrics Society.
📖
(18 May 2024 ~ Nature: Communications)
‘Cerebral microstructural alterations in Post-COVID-condition are related to cognitive impairment, olfactory dysfunction and fatigue’.
➤
‘xxx’
© 2024
Hosp
et al
/
Nature: Communications.
📖
(6 Aug 2024 ~ MedPage Today)
‘Three Years After COVID Hospitalization, Cognitive Problems Persist and Worsen’.
➤
‘xxx’
© 2024
Judy George
/
MedPage Today.
📖
(10 Jul 2024 ~ Nature: Aging)
‘Tracking cognitive trajectories in older survivors of COVID-19 up to 2.5 years post-infection’.
➤
‘xxx’
© 2024
Liu
et al
/
Nature: Aging.
📖
(22 Jan 2025 ~ JAMA Network: Infectious Diseases)
‘Sex Differences in Long COVID’.
➤
‘In this cohort study of 12,276 individuals,
females had a
significantly higher risk
of long COVID compared with males after adjusting for sociodemographic and clinical risk factors.
The sex-based difference in long COVID risk was age, pregnancy, and menopause dependent, with the
highest risk among females
aged
40 to
55 years.’
© 2025
Shah
et al
/
JAMA Network: Infectious Diseases.
📖
(17 Aug 2024 ~ Journal of Neuroinflammation)
‘Deterioration of neuroimmune homeostasis in Alzheimer’s Disease patients who survive a COVID-19 infection’.
➤
‘xxx’
© 2024
Villareal
et al
/
Journal of Neuroinflammation.
📖
(13 Dec 2023 ~ JAMA Network)
‘Long COVID in Nursing Home Residents Manifests as Functional Decline’.
➤
‘xxx’
© 2023
Emily Harris
/
JAMA Network.
📖
(6 Feb 2024 ~ The Lancet: Preprint)
‘Temporal Association between COVID-19 Infection and Subsequent New-Onset Dementia in Older Adults: A Systematic Review and Meta-Analysis’.
➤
‘xxx’
© 2024
Shan
et al
/
The Lancet: Preprint.
📖
(13 Sep 2024 ~ Elsevier: Ageing Research Reviews)
‘The risk of cognitive decline and dementia in older adults diagnosed with COVID-19: A systematic review and meta-analysis’.
➤
‘xxx’
© 2024
Shrestha
et al
/
Elsevier: Ageing Research Reviews.
📖
(15 Aug 2024 ~ Heliyon)
‘Brain effects of mild COVID-19 in healthy young adults: A pilot study’.
➤
‘xxx’
© 2024
Lipton
et al
/
Heliyon.
📖
(22 Nov 2024 ~ Annals of Neurology)
‘Neurologic Manifestations of Long COVID Disproportionately Affect Young and Middle-Age Adults’.
➤
‘Younger and middle-age individuals are disproportionally affected by Neuro-PASC regardless of acute COVID-19 severity.
Although older people more frequently have abnormal neurologic findings and comorbidities, younger and middle-age patients suffer from a higher burden of Neuro-PASC symptoms and cognitive dysfunction contributing to decreased quality of life.
Neuro-PASC principally affects adults in their prime.’
© 2024
Choudhury
et al
/
Annals of Neurology.
📖
(29 Jun 2023 ~ The Lancet ~ Regional Health: Europe)
‘Shedding light on the work burden of long COVID’.
➤
‘xxx’
© 2023
Lemogne & Pitron
/
The Lancet: Regional Health (Europe).
‘Venus lamenting the death of Adonis’, after Benjamin West (1771).
‘The strongest body shall it make most weak,
Strike the wise dumb and teach the fool to speak...
It shall be raging mad and silly mild,
Make the young old, the old become a child.’
From
‘Venus and Adonis’, by William Shakespeare (1593).
📖
(18 May 2023 ~ Frontiers in Neurology)
‘COVID-19 and neurological disorders: what might connect Parkinson’s disease to SARS-CoV-2 infection’.
➤
‘xxx’
© 2023
Iacono
et al
/
Frontiers in Neurology.
📖
(10 Jan 2022 ~ Elsevier: Case Report)
‘Parkinsonism: An emerging post-COVID sequelae’.
➤
‘xxx’
© 2022
Rao
et al
/
Elsevier: Case Report.
📖
(22 Sep 2022 ~ Nature: Medicine)
‘Long-term neurologic outcomes of COVID-19’.
➤
‘xxx’
© 2022
Xu, Xie & Al-Aly
/
Nature: Medicine.
📖
(19 Aug 2024 ~ Yale Medicine)
‘Long COVID Symptoms: Internal Tremors and Vibrations’.
➤
‘xxx’
© 2024
Lisa Sanders /
Yale Medicine.
📖
(6 Aug 2022 ~ The Lancet)
‘Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study’.
➤
‘xxx’
© 2022
Ballering
et al
/
The Lancet.
📖
(28 Feb 2024 ~ The New England Journal of Medicine)
‘Long Covid and Impaired Cognition — More Evidence and More Work to Do’.
➤
‘xxx’
© 2024
Al-Aly & Rosen
/
The New England Journal of Medicine.
📖
(5 Jul 2023 ~ The Lancet ~ Regional Health: Western Pacific)
‘Post-COVID cognitive dysfunction: current status and research recommendations for high risk population’.
➤
‘xxx’
© 2023
Quan
et al
/
The Lancet: Regional Health (Western Pacific).
📖
(30 Jan 2025 ~ Nature: Medicine)
‘Plasma proteomic evidence for increased β-amyloid pathology after SARS-CoV-2 infection’.
➤
‘xxx’
© 2025
Duff
et al
/
Nature: Medicine.
📖
(29 Jun 2023 ~ Nature: Cell Death Discovery)
‘Long-term effects of SARS-CoV-2 infection on human brain and memory’.
➤
‘xxx’
© 2023
Ding & Zhao
/
Nature: Cell Death Discovery.
📖
(19 Jun 2023 ~ The Lancet: Preprint)
‘Vagus Nerve Dysfunction in the Post-COVID-19 Condition’.
➤
‘xxx’
© 2023
Lladós
et al
/
The Lancet: Preprint.
📖
(10 Nov 2023 ~ Bloomberg UK)
‘Covid Loss of Smell Takes Up to Three Years to Return, Study Finds’.
➤
‘xxx’
© 2023
Jason Gale
/
Bloomberg UK.
📖
(1 Nov 2022 ~ Cell Reports)
‘SARS-CoV-2 infects neurons and induces neuroinflammation in a non-human primate model of COVID-19’.
➤
‘xxx’
© 2022
Beckman
et al
/
Cell Reports.
📖
(17 Aug 2024 ~ Nature: Scientific Reports)
‘Patients recovering from COVID-19 who presented with anosmia during their acute episode have behavioral, functional, and structural brain alterations’.
➤
‘xxx’
© 2024
Kausel
et al
/
Nature: Scientific Reports.
📖
(14 Aug 2024 ~ Nature: Aging)
‘Proteomics identifies potential immunological drivers of postinfection brain atrophy and cognitive decline’.
➤
‘xxx’
© 2024
Duggan
et al
~
Nature: Aging.
📖
(27 Feb 2023 ~ The Lancet: eClinicalMedicine)
‘Structural brain changes in patients with post-COVID fatigue: a prospective observational study’.
➤
‘xxx’
© 2023
Heine
et al
/
The Lancet: eClinicalMedicine.
📖
(15 Dec 2022 ~ Nature)
‘SARS-CoV-2 infection and persistence in the human body and brain at autopsy’.
➤
‘xxx’
© 2022
Stein
et al
/
Nature.
📖
(19 Aug 2024 ~ Technology Networks: Immunology & Microbiology)
‘New Study Links Long COVID to Brain Inflammation and Low Cortisol Levels’.
➤
‘COVID-19 proteins remain in the brain long after infection, causing cortisol levels to drop and the nervous system to become inflamed.
Reduced cortisol may trigger overreactions to stressors, leading to long COVID symptoms like fatigue, depression, and brain fog.’
© 2024
University of Colorado
/
Technology Networks: Immunology & Microbiology.
📖
(23 May 2023 ~ PNAS)
‘Brain imaging and neuropsychological assessment of individuals recovered from a mild to moderate SARS-CoV-2 infection’.
➤
‘xxx’
© 2023
Petersen
et al
/
PNAS.
📖
(5 May 2023 ~ Neurology Journals)
‘Deep Phenotyping of Neurologic Post-Acute Sequelae of SARS-CoV-2 Infection’.
➤
‘xxx’
© 2023
Mina
et al
/
Neurology Journals.
📖
(4 Jul 2024 ~ Science Alert)
‘COVID’s Hidden Toll: Full-Body Scans Reveal Long-Term Immune Effects’.
➤
‘xxx’
© 2024
Carly Cassella
/
Science Alert.
📖
(11 Jan 2024 ~ Nature Immunology)
‘Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2’.
➤
‘xxx’
© 2024
Yin
et al
/
Nature Immunology.
📖
(15 Mar 2024 ~ Science News)
‘Long COVID brain fog may be due to damaged blood vessels in the brain’.
➤
‘xxx’
© 2024
Meghan Rosen
/
Science News.
📖
(22 Feb 2024 ~ Nature: Neuroscience)
‘Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment’.
➤
‘xxx’
© 2024
Greene
et al
/
Nature: Neuroscience.
📖
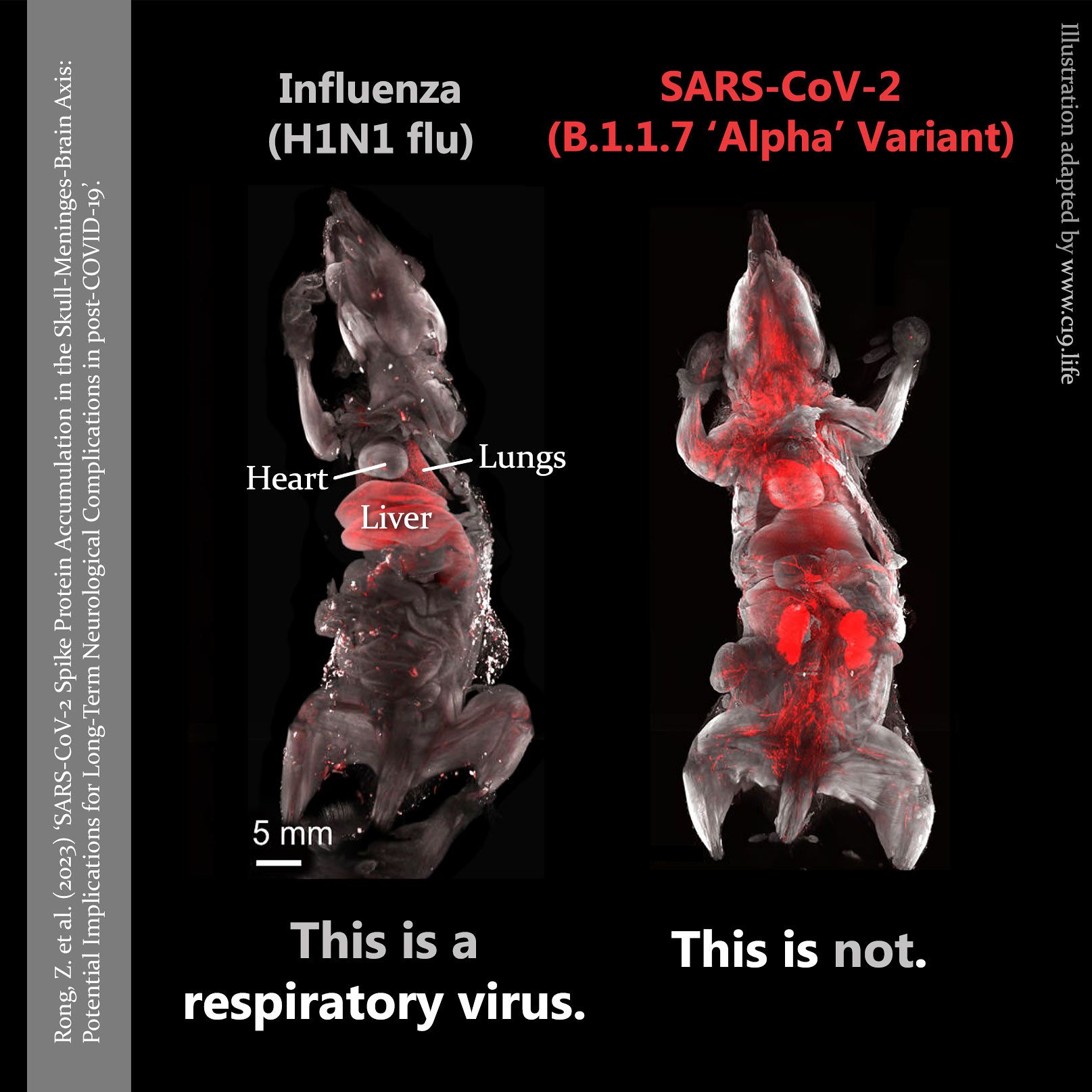
(29 Nov 2024 ~ Cell Host & Microbe)
‘Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19’.
➤
‘xxx’
© 2024
Rong
et al
/
Cell Host & Microbe.
📖
(18 Apr 2023 ~ Trends in Endocrinology & Metabolism)
‘Long COVID: pathophysiological factors and abnormalities of coagulation’.
➤
‘xxx’
© 2023
Turner
et al
/
Trends in Endocrinology & Metabolism.
📖
(4 Nov 2024 ~ Bloomberg UK)
‘Unraveling Covid’s Pernicious Role in Brain Fog and Clotting’.
➤
‘xxx’
© 2024
Jason Gale
/
Bloomberg UK.
📖
(26 Dec 2024 ~ Bloomberg UK)
‘Covid Pregnancies May Have Boosted Autism Risk, Study Shows’.
➤
‘Exposure to the virus
in utero may have affected children’s development, according to a UCLA study, adding to a list of health problems emerging in the wake of the global pandemic.’
© 2024
Jason Gale
/
Bloomberg UK.
📖
(9 Jul 2020 ~ Nature: NPJ Parkinson’s Disease)
‘Current and projected future economic burden of Parkinson’s disease in the U.S.’
➤
‘xxx’
© 2020
Yang
et al
/
Nature: NPJ Parkinson’s Disease.
📖
(12 Mar 2022 ~ The Lancet: eClinicalMedicine)
‘Global and regional spending on dementia care from 2000–2019 and expected future health spending scenarios from 2020–2050: An economic modelling exercise’.
➤
‘xxx’
© 2022
Pedroza
et al
/
The Lancet: eClinicalMedicine.
📖
(22 Jan 2025 ~ The Journal of Infectious Diseases)
‘The Current and Future Burden of Long COVID in the United States’.
➤
‘xxx’
© 2025
Bartsch
et al
/
The Journal of Infectious Diseases.
📖
(8 Jan 2022 ~ Brain, Behavior, and Immunity)
‘Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis’.
➤
‘xxx’
© 2022
Ceban
et al
/
Brain, Behavior, and Immunity.
More... Brain & Nervous System
by C19.Life... et al
•
21 November 2025
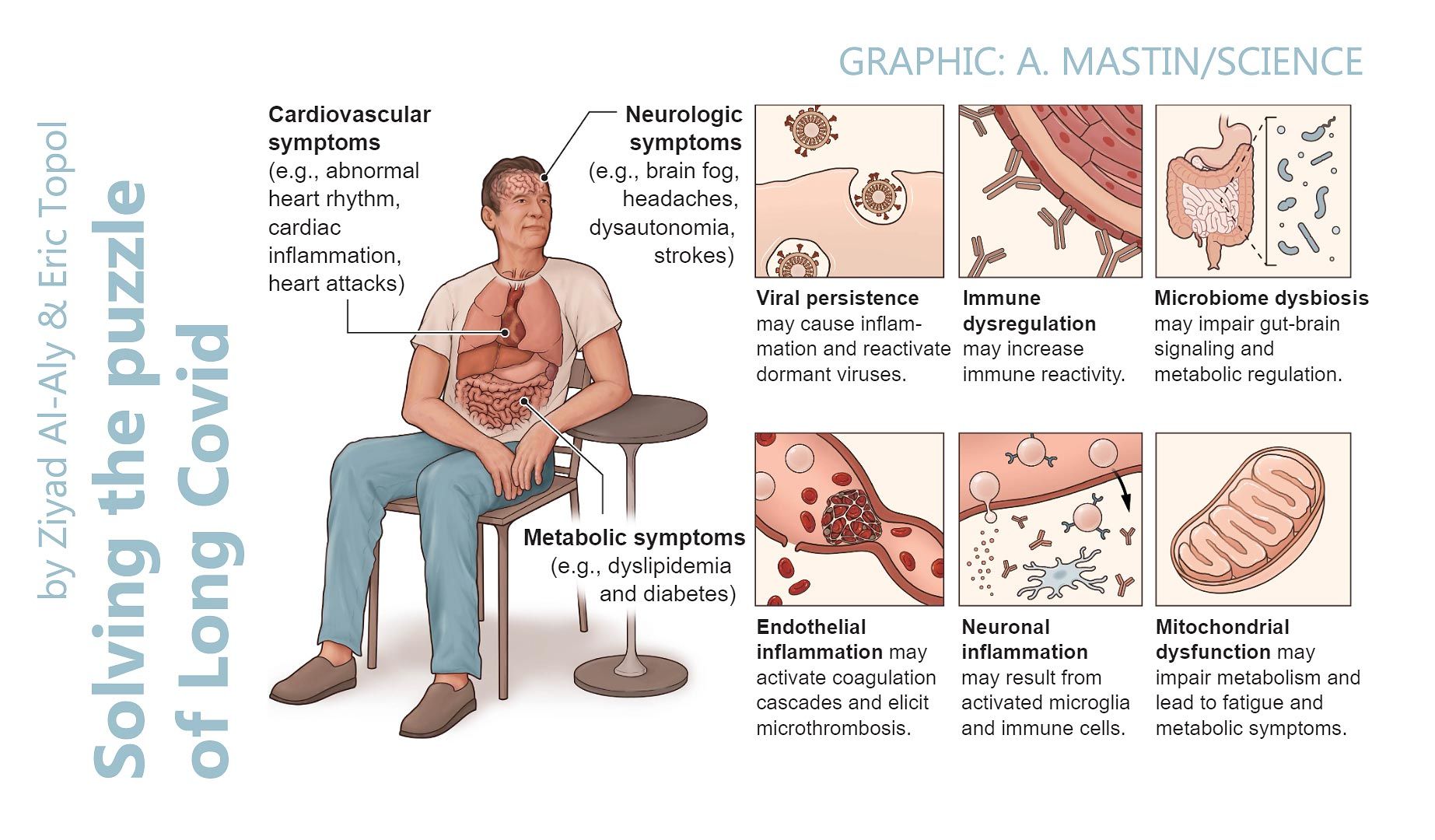
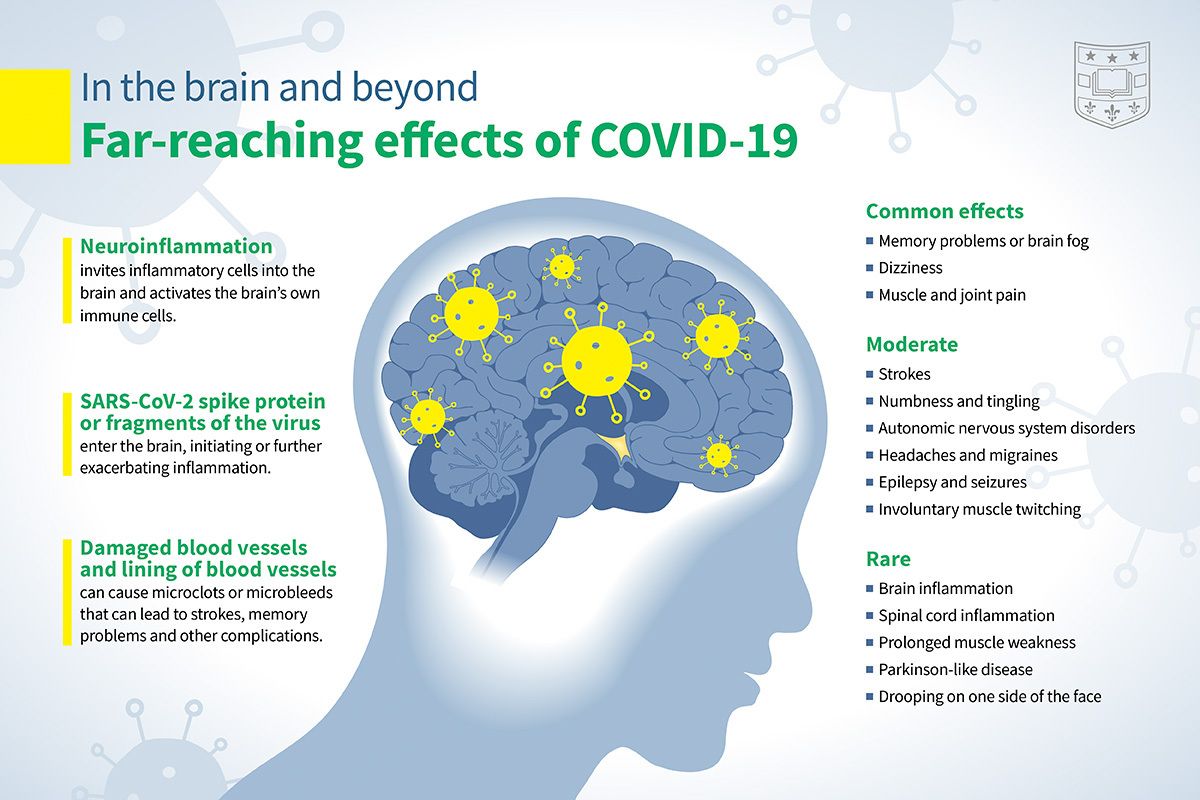
‘Although COVID-19 was originally considered a respiratory illness, it is now well established that SARS-CoV-2 infection can have far-reaching impacts on the nervous system. Common neurological symptoms in Long COVID [PASC] include new-onset cognitive difficulties, dysautonomia, fatigue, and peripheral neuropathy.’ from ‘Neuroimmune pathophysiology of long COVID’ by Moen et al / Psychiatry and Clinical Neurosciences (2025).
by Byrne et al ~ Nature Pediatric Research / Bioengineer
•
11 November 2025
‘The pediatric population, once thought to be relatively spared from severe outcomes, has presented with significant neurological manifestations that raise concerns about the short- and long-term effects of SARS-CoV-2 on the developing nervous system.’
by David Putrino ❂ Sonya Buyting ~ Radio-Canada / Canadian Broadcasting Corporation
•
20 March 2025
CBC Radio-Canada interview with long COVID [PASC] researcher David Putrino from the Icahn School of Medicine at Mount Sinai in New York.
by Jason Gale / Bloomberg UK
•
3 March 2025
‘For patients already battling Alzheimer’s disease, studies indicate that Covid can exacerbate brain inflammation, damage immune cells, and accelerate the disease. Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection. Mild Covid cases in younger adults have also been linked to brain issues affecting memory and thinking. ’
by News Medical Life Sciences ❂ Duff et al / Nature Medicine
•
2 February 2025
‘Scientists discover that even mild COVID-19 can alter brain proteins linked to Alzheimer’s disease, potentially increasing dementia risk. COVID-19-positive individuals exhibited lower cognitive test performance compared to controls – equivalent to almost two years of age-related cognitive decline. ’
by R. Peter et al / PLOS Medicine
•
23 January 2025
‘The predominant symptoms, often clustering together, remain fatigue, cognitive disturbance and chest symptoms, including breathlessness, with sleep disorder and anxiety as additional complaints. Many patients with persistent PCS [PASC/‘Long Covid’] show impaired executive functioning, reduced cognitive processing speed and reduced physical exercise capacity.’
by Greene et al / Nature: Neuroscience [Commentary by Danielle Beckman]
•
22 February 2024
❦ “This study confirms everything that I have seen in the microscope over the last few years. The authors of the study use a technique called dynamic contrast-enhanced magnetic resonance imaging ( DCE-MRI ), an imaging technique that can measure the density , integrity , and leakiness of tissue vasculature. Comparing all individuals with previous COVID infection to unaffected controls revealed decreased general brain volume in patients with ‘brain fog’ – along with significantly reduced cerebral white matter volume in both hemispheres in the recovered and ‘brain fog’ cohorts . Covid-19 induces brain-volume loss and leaky blood-brain barrier in some patients. How can this be more clear?” © 2024 Dr. Danielle Beckman, Neuroscientist (PhD Biological Chemistry) ➲ ❂ 📖 (22 Feb 2024 ~ Nature: Neuroscience) Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment ➤ ‘ Our data suggest that sustained systemic inflammation and persistent localized blood-brain barrier (BBB) dysfunction is a key feature of long COVID-associated brain fog. Patients with long COVID had elevated levels of IL-8, GFAP and TGFβ, with TGFβ specifically increased in the cohort with brain fog. GFAP is a robust marker of cerebrovascular damage and is elevated after repetitive head trauma, reflecting BBB disruption, as seen in contact sport athletes and in individuals with self-reported neurological symptoms in long COVID. Interestingly, TGFβ was strongly associated with BBB disruption and structural brain changes. ’ [Layperson overview] 📖 (February 2024 ~ Genetic Engineering and Biotechnology News) Leaky Blood Vessels in the Brain Linked to Brain Fog in Long COVID Patients ➤ [Related] 📖 (7 Feb 2022 ~ Nature: Cardiovascular Research) Blood–brain barrier link to human cognitive impairment and Alzheimer’s disease ➤ ❂
by Dr. David Joffe PhD / FRACP (Respiratory Physician)
•
27 January 2024
❦ “It’s really not in the interest of the virus to kill us quickly. That’s why it has mutated to immune escape. That way it enters silently, and then eats you slowly whilst you’re still a spreading vector. Refrigerator trucks are long gone. That’s all the political class wanted. The unseen costs of CVD [cardiovascular disease] , DM [diabetes mellitus] , and both dementia and Parkinson’s Disease are the train coming down the tunnel. The economists are catching up. The actuaries are already there. Politicians and most people? Not yet...” ❂ © 2024 Dr. David Joffe PhD / FRACP (Respiratory Physician) ➲
by Scardua-Silva et al / Nature: Scientific Reports
•
19 January 2024
❦ ‘Although some studies have shown neuroimaging and neuropsychological alterations in post-COVID-19 patients, fewer combined neuroimaging and neuropsychology evaluations of individuals who presented a mild acute infection. Here we investigated cognitive dysfunction and brain changes in a group of mildly infected individuals. We conducted a cross-sectional study of 97 consecutive subjects ( median age of 41 years ) without current or history of psychiatric symptoms (including anxiety and depression) after a mild infection , with a median of 79 days (and mean of 97 days ) after diagnosis of COVID-19. We performed semi-structured interviews, neurological examinations, 3T-MRI scans, and neuropsychological assessments. The patients reported memory loss ( 36% ), fatigue ( 31% ) and headache ( 29% ). The quantitative analyses confirmed symptoms of fatigue ( 83% of participants), excessive somnolence ( 35% ), impaired phonemic verbal fluency ( 21% ), impaired verbal categorical fluency ( 13% ) and impaired logical memory immediate recall ( 16% ). Our group… presented higher rates of impairments in processing speed ( 11.7% in FDT- Reading and 10% in FDT- Counting ). The white matter (WM) analyses with DTI * revealed higher axial diffusivity values in post-infected patients compared to controls. * Diffusion tensor imaging tractography , or DTI tractography, is an MRI (magnetic resonance imaging) technique most commonly used to provide imaging of the brain. Our results suggest persistent cognitive impairment and subtle white matter abnormalities in individuals mildly infected , without anxiety or depression symptoms. One intriguing fact is that we observed a high proportion of low average performance in our sample of patients (which has a high average level of education ), including immediate and late verbal episodic memory, phonological and semantic verbal fluency, immediate visuospatial episodic memory, processing speed, and inhibitory control . Although most subjects did not present significant impaired scores compared with the normative data, we speculate that the low average performance affecting different domains may result in a negative impact in everyday life , especially in individuals with high levels of education and cognitive demands .’ ❂ ❦ Note how these findings might negatively affect daily activities that demand sustained cognitive attention and fast reaction times – such as driving a car or motorbike, or piloting a plane. Consider air-traffic control. Consider the impact on healthcare workers whose occupations combine long periods of intense concentration with a need for critical precision. ❂ 📖 (19 Jan 2024 ~ Nature: Scientific Reports) Microstructural brain abnormalities, fatigue, and cognitive dysfunction after mild COVID-19 ➤ © 2024 Nature .
by Shajahan et al / Frontiers in Aging Neuroscience
•
8 January 2024
‘[COVID-19’s] ability to invade the central nervous system through the hematogenous and neural routes, besides attacking the respiratory system, has the potential to worsen cognitive decline in Alzheimer’s disease patients. The severity of this issue must be highlighted.’
by Lady Chuan
•
5 December 2023
❦ Always Covid+ Colleague: — “One of the medical groups. One of the groups. One of the groups...” Moderator: — “Is there something you want to share?” Always Covid+ Colleague: — “I was asked something. I don’t know. It has something to do with something.” This is what Covid is doing to the brain. Unfortunately this is not an isolated incident – but something I’m witnessing all day long throughout the company. ❂ © 2023 Lady Chuan ➲
by Martin et al / Journal of Neurology
•
7 November 2023
❦ ‘It is now well established that post-COVID syndrome ( PCS ) represents a serious complication in a substantial number of patients following SARS-CoV-2 infection. PCS is diagnosed when COVID-19-related symptoms persist for more than 3 months. It can occur even after an initially mild to moderate course of infection , and comprises a large variety of symptoms . Around 30% of PCS patients show neurological and neuropsychiatric sequelae , such as fatigue , depressive symptoms , and cognitive dysfunction . These are experienced as particularly debilitating, as they have detrimental effects on daily functioning in PCS patients and hamper a successful return to their jobs. Fatigue is a frequent and one of the most debilitating symptoms in post-COVID syndrome (PCS). Recently, we proposed that fatigue is caused by hypoactivity of the brain’s arousal network and reflected by a reduction of cognitive processing speed . Eighty-eight PCS patients with cognitive complaints and 50 matched healthy controls underwent neuropsychological assessment. Seventy-seven patients were subsequently assessed at 6-month follow-up. Patients showed cognitive slowing indicated by longer reaction times compared to control participants in a simple-response tonic alertness task and in all more complex tasks requiring speeded performance . Reduced alertness correlated with higher fatigue . Alertness dysfunction remained unchanged at 6-month follow-up and the same was true for most attention tasks and cognitive domains .’ ❂ 📖 (7 Nov 2023 ~ Journal of Neurology) Persistent cognitive slowing in post-COVID patients: longitudinal study over 6 months ➤ © 2023 Journal of Neurology .
by Rich Haridy / New Atlas
•
31 October 2023
A layperson-level overview from New Atlas on how all variants of SARS-CoV-2 – the virus that causes COVID-19 – are ‘neuroinvasive’ , meaning that all can infect or enter the brain and the nervous system . (From July 2023 Nature Communications study: ‘Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants’.)
by Outbreak Updates
•
11 October 2023
❦ Your brain is a vast city. The roads (myelin) in this city let cars move efficiently. Oligodendrocytes are the construction workers who maintain these roads. As we age, these workers slow down, causing traffic jams and slower thoughts. Enter SARS-CoV-2, the destructive rioter. It doesn’t just disrupt traffic; it damages the roads and chases away the construction crews. Weeks after the riot, the city still struggles to function, with long-lasting road damages and traffic jams. This is the ‘brain fog’ of post-COVID life. ❂ 📖 (24 Sep 2023 ~ Aging and Disease) Role of Microglia, Decreased Neurogenesis and Oligodendrocyte Depletion in Long COVID-Mediated Brain Impairments ➤ © 2023 Outbreak Updates ➲
by Sauve et al / eBioMedicine: Lancet Discovery Science
•
12 September 2023
❦ ‘We have recently demonstrated a causal link between loss of gonadotropin-releasing hormone ( GnRH ), the master molecule regulating reproduction , and cognitive deficits during pathological aging , including Down syndrome and Alzheimer’s disease. Olfactory and cognitive alterations , which persist in some COVID-19 patients, and long-term hypotestosteronaemia in SARS-CoV-2-infected men are also reminiscent of the consequences of deficient GnRH, suggesting that GnRH system neuroinvasion could underlie certain post-COVID symptoms and thus lead to accelerated or exacerbated cognitive decline . We explored the hormonal profile of COVID-19 patients and targets of SARS-CoV-2 infection in post-mortem patient brains and human fetal tissue. We found that persistent hypotestosteronaemia in some men could indeed be of hypothalamic origin , favouring post-COVID cognitive or neurological symptoms , and that changes in testosterone levels and body weight over time were inversely correlated. Infection of olfactory sensory neurons and multifunctional hypothalamic glia called tanycytes highlighted at least two viable neuroinvasion routes . Furthermore, GnRH neurons themselves were dying in all patient brains studied , dramatically reducing GnRH expression. Human fetal olfactory and vomeronasal epithelia , from which GnRH neurons arise, and fetal GnRH neurons also appeared susceptible to infection . Putative GnRH neuron and tanycyte dysfunction following SARS-CoV-2 neuroinvasion could be responsible for serious reproductive , metabolic , and mental health consequences in long-COVID and lead to an increased risk of neurodevelopmental and neurodegenerative pathologies over time in all age groups .’ ❂ 📖 (12 Sep 2023 ~ eBioMedicine: Lancet Discovery Science) Long-COVID cognitive impairments and reproductive hormone deficits in men may stem from GnRH neuronal death ➤ © 2023 eBioMedicine: Lancet Discovery Science .
by Di Chiara et al / Acta Paediatrica
•
9 September 2023
❦ Children have largely been unaffected by severe COVID-19 compared to adults, but data suggest that they may have experienced new conditions after developing the disease. We compared 1656 exposed and 1656 unexposed children from 1 February 2020 to 30 November 2021. We found significantly higher risks for some new conditions in exposed children, including mental health issues and neurological problems . The overall excess risk for new-onset conditions after COVID-19 was 78% higher in the exposed than unexposed children. ❂ 📖 (9 Sep 2023 ~ Acta Paediatrica) Comparative study showed that children faced a 78% higher risk of new-onset conditions after they had COVID-19 ➤ © 2023 Di Chiara et al / Acta Paediatrica.
by Dr. Sean Mullen
•
25 August 2023
❦ “When someone shows a severe personality shift, there could be many reasons. One possibility? Their brain may have been affected by COVID-19. It’s crucial to approach with empathy, to consider all potential causes, and to consult healthcare professionals. Don’t jump to conclusions, but stay informed.” © 2023 Dr. Sean Mullen . ➲
by Martinez-Marmol & Hilliard / Queensland Brain Institute
•
8 June 2023
❦ Researchers at The University of Queensland have discovered viruses such as SARS-CoV-2 can cause brain cells to fuse, initiating malfunctions that lead to chronic neurological symptoms. SARS-CoV-2, the virus that causes COVID-19, has been detected in the brains of people with 'Long COVID' months after their initial infection. "We discovered COVID-19 causes neurons to undergo a cell fusion process, which has not been seen before," Professor Hilliard said. "After neuronal infection with SARS-CoV-2, the spike S protein becomes present in neurons, and once neurons fuse, they don't die." "They either start firing synchronously, or they stop functioning altogether." As an analogy, Professor Hilliard likened the role of neurons to that of wires connecting switches to the lights in a kitchen and a bathroom. "Once fusion takes place, each switch either turns on both the kitchen and bathroom lights at the same time, or neither of them," he said. "It's bad news for the two independent circuits." The discovery offers a potential explanation for persistent neurological effects after a viral infection. "In the current understanding of what happens when a virus enters the brain, there are two outcomes – either cell death or inflammation," Dr Martinez-Marmol said. "But we've shown a third possible outcome, which is neuronal fusion." Dr Martinez-Marmol said numerous viruses cause cell fusion in other tissues, but also infect the nervous system and could be causing the same problem there. "These viruses include HIV, rabies, Japanese encephalitis, measles, herpes simplex virus and Zika virus," he said. “Our research reveals a new mechanism for the neurological events that happen during a viral infection. “This is potentially a major cause of neurological diseases and clinical symptoms that is still unexplored.” ❂ 📖 (7 June 2023 ~ Science Advances) SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity ➤ 📖 (8 June 2023 ~ Queensland Brain Institute) COVID-19 can cause brain cells to 'fuse' ➤ © 2023 Martinez-Marmol & Hilliard / Queensland Brain Institute / University of Queensland.
by NHS Palliative Medicine Consultant
•
20 May 2023
❦ “A bizarre recurring point of debate: — “People die every day of lots of other things!” True, but you don’t catch a stroke from other people in a restaurant. ” © 2023 NHS Palliative Medicine Consultant .
by NHS Palliative Medicine Consultant
•
19 May 2023
❦ “What if Covid has been causing mass cognitive impairment and we are all living in an increasingly stupid society? Mad things could happen with that: imagine if hospitals got rid of masks or people started to believe Covid was just a cold? I know that’s far-fetched, but imagine!” ❂ © 2023 NHS Palliative Medicine Consultant .
by Conor Browne
•
8 May 2023
❦ ‘A significant part of my professional role is forecasting: that is to say, quantifying the risks faced by commercial and other organisations in the future as a result of SARS-CoV-2 and other pathogens (especially H5N1). As such, I often produce bespoke scenarios for clients – 6 months, 12 months, 24 months into the future – assigning probabilities to each scenario occurring. As this article * makes clear, the risk of the emergence of a new Variant of Concern (VOC) within the next two years is about 20 percent. * 📖 (5 May 2023 ~ CNN) Covid-19 experts say they warned White House about chance of an Omicron-level event within the next two years ➤ Any risk manager reading this will know that this is a highly significant risk. Biological risks do not exist in isolation; rather, they are nested within both the domestic politics of any given jurisdiction, and within geopolitics in general. This is a very important point to remember. The recent declaration by the WHO * has (rightfully) angered many people – but, frankly, it has made little practical difference to what I do professionally. * 📖 (5 May 2023 ~ CNN) WHO says Covid-19 is no longer a global health emergency ➤ The vast majority of national governments essentially stopped addressing C-19 in any serious manner quite some time ago. This is the key domestic political risk that intersects with the biological risk of the emergence of a new VOC. National apathy regarding C-19, combined with the growing mainstreaming of both anti-vax sentiment and a reduction in infection control measures in general (such as dropping respirator use in healthcare environments), has created a very dangerous situation. In short, as a global society, we are less prepared now for either the emergence of another disease with pandemic potential (specifically H5N1 avian influenza), or the emergence of a SARS-CoV-2 VOC that exhibits significant immune evasion around current vaccines, than we were in 2019. If either – or both – of these were to occur within the next couple of years, we would be in deep, deep trouble. Currently, we are allowing SARS-CoV-2 to transmit entirely unchecked; this means that pressures on healthcare systems globally will inexorably continue to increase. Concurrently, the population of many jurisdictions worldwide are now primed to reject even the lightest of societal non-pharmaceutical interventions (NPIs) [ such as respirator/mask mandates ] . This combination virtually guarantees that should an immune-evasive VOC emerge we would see healthcare system collapse in many jurisdictions. The short-term goals of domestic politics (maintaining or attaining political power) relies on shying away from the discussion of anything to do with the pandemic. This is the tragic ground truth that has a high chance of coming back to bite us all very badly soon.’ © 2023 Conor Browne . ➲
by Herrera et al / Nature: Scientific Reports
•
19 April 2023
❦ The results presented here reveal that at least 85% [of the 214 patients with post COVID-19 syndrome] exhibit deficits in one neuropsychological test . Also, the youngest patients were those who showed the most marked and heterogeneous cognitive impairment , while the oldest patients maintained their cognitive functions preserved to a greater extent with only a mild impairment in attention and speed processing. ❂ 📖 (19 Apr 2023 ~ Nature: Scientific Reports) Cognitive impairment in young adults with post COVID-19 syndrome ➤ © 2023 Herrera et al / Nature.
by Linseman Laboratory / University of Denver
•
4 April 2023
❦ The Linseman Laboratory is studying the long-term brain health effects of COVID-19 in individuals with and without traumatic brain injury (TBI). Preliminary data suggest that those with a history of both COVID-19 and TBI experience more severe Long COVID symptoms, a higher symptom burden , and more frequent symptoms . Those who reported having COVID-19 and TBI reported worse depressive symptoms , worse functional outcomes , and increased fatigue . ❂ 📖 (4 Apr 2023 ~ SciTechDaily) Researchers Discover Connection Between Traumatic Brain Injury and Long COVID ➤ © 2023 Linesman Laboratory / University of Denver / SciTechDaily.
by EurekAlert / Journal of Alzheimer’s Disease Reports
•
4 April 2023
‘All subtypes of dementia, irrespective of patients’ previous dementia types, behaved like rapidly progressive dementia following COVID-19 [infection with SARS-CoV-2] .’
by J.P.S Peron / Human Genetics
•
31 March 2023
❦ From mild anosmia to severe ischemic stroke , the impact of SARS-CoV-2 on the central nervous system is still a great challenge to scientists and healthcare practitioners. Besides the acute and severe neurological problems described, as encephalopathies , leptomeningitis , and stroke , the chronic impact observed during Long COVID or the post-acute sequelae of COVID-19 (PASC) greatly intrigues scientists worldwide. Strikingly, even asymptomatic , and mild-diseased patients may evolve with important neurological and psychiatric symptoms such as confusion , memory loss , cognitive decline and chronic fatigue , associated or not with anxiety and depression . ❂ 📖 (1 Apr 2023 ~ Human Genetics) Direct and indirect impact of SARS-CoV-2 on the brain ➤ © 2023 J.P.S Peron / Human Genetics.
by Palermo et al / Brain Science
•
23 March 2023
❦ The possible neurological consequences of SARS-CoV-2 infection, associated with physical and cognitive frailty, could lead to a worsening of Parkinson’s disease (PD) in infected patients or – more rarely – to an increase in the Parkinsonian symptomatology . Parkinson’s disease (PD) or Parkinsonism has been described after infections with viruses , such as the Epstein-Barr virus , hepatitis C virus , HIV , influenza A virus , Japanese encephalitis virus , varicella zoster virus , or West Nile virus . Therefore, the hypothesis that SARS-CoV-2 may have even longer-term effects on the brain and lead to an increase in cases of Parkinson’s disease, as occurred in the years following the Spanish flu , has been put forward. ❂ 📖 (23 Mar 2023 ~ Brain Science) Parkinson’s Disease, SARS-CoV-2, and Frailty: Is There a Vicious Cycle Related to Hypovitaminosis D? ➤ © 2023 Palermo et al / Brain Science.
by Vernon et al / WORK: A Journal of Prevention, Assessment & Rehabilitation
•
7 March 2023
‘Low and medium physical and cognitive exertion triggered PEM for both Long COVID respondents and ME/CFS patients. Long COVID respondents indicated that high physical and cognitive exertion, stress, food or chemical sensitivities, temperature extremes, insufficient sleep, and illness were significantly more likely to trigger PEM than reported by ME/CFS patients.’
by E. Wesley Ely / Stat
•
16 February 2023
❦ It's no wonder that depression and PTSD rates ✢ are up in people living with Long COVID. ✢ Long COVID: major findings, mechanisms and recommendations ➤ There are no approved therapies for the physical or cognitive disabilities that now plague 65 million people around the world, a conservative estimate given the degree of undocumented cases. It is now clear from US and UK investigations of approximately 2,000 previously hospitalized Covid patients that six months later more than half have problems managing finances and paying bills as well as completing everyday activities like preparing meals, bathing, getting dressed, or walking across a room. But what exactly is going on inside the brains of these people from a biological and pathological perspective? Autopsy studies show that the virus can persist ✢ in some people for many months even though they have no symptoms and test negative for the virus. ✢ Persistent SARS-CoV-2 infection in patients seemingly recoveredfrom COVID-19 ➤ Brains donated by people who died of Covid-19 also show widespread problems in the cells lining the blood vessels and exaggerated clotting, supporting the idea of Covid-19 as a blood flow disorder ✢ that brings on brain disease. ✢ Neurovascular injury with complement activation and inflammation in COVID-19 ➤ Perhaps the most harrowing thing I have done in 30 years as a physician-scientist has been to ask family members I'd never met, often in the middle of the night via telephone during the height of the Covid surges, if I and my colleagues could study their loved one's brain. In a study we conducted of 20 of these priceless brain donations ✢ , we found brain swelling due to decreased blood flow and heightened activity in microglial cells, the so-called 'white matter' in brains that support the neurons that transmit thoughts and help store information. We saw this even in young previously healthy individuals. ✢ Brain autopsies of critically ill COVID-19 patients demonstrate heterogeneous profile of acute vascular injury, inflammation and age-linked chronic brain diseases ➤ A study from the National Institutes of Health of 44 complete autopsies ✢ mapped and quantified the distribution of SARS-CoV-2 and showed it was widely distributed throughout the body, including in the hypothalamus and cerebellum in the brain and neurons in the spinal cord. ✢ SARS-CoV-2 infection and persistence in the human body and brain at autopsy ➤ Especially relevant to Long Covid, viral fragments were detected in some of the brains of people who died many months after symptom onset. In Their Own Words Barbara Nivens, who retired from retail management at age 59, has been diagnosed by her neurologist as having rapid onset dementia due to Covid-19. An incredibly thorough medical work-up found no plausible causes for this dementia other than its onset following her Covid infection, which she contracted before the vaccine was available. Matt Fitzgerald, age 26, is a mechanical engineer who worked for Tesla and now designs surgical devices – when he can. Since recovering from his initial bout with Covid-19, he's developed a condition characteristic of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) known as post-exertional malaise, which is why even slight exertion leaves him and millions like him inexplicably incapacitated. ❦ Barbara Nivens: — “I walk down the hall and see dozens of pictures of family trips and feel like a ghost because I don't remember any of them. Now I'm trying to figure out who Barbara 2.0 is going to be.” (Her husband, tearing up as he listened to her, said softly, “I just want my wife back.”) ❦ Matt Fitzgerald: — “I feel like I'm underwater. When you talk to me, I can hear you, but my brain does not understand the words. I can't comprehend what you're saying. I have no intellectual capacity or energy to digest data. At work my brain is just begging for rest. I struggle with finding words and completing tasks in a timely manner. It's the worst. I'll be in a meeting and know exactly what I want to say before I say it. I'll start saying it and I'll get to a word, and I just cannot think of the word. I'll just be like, ‘Give me a moment,’ and I'll go through my brain cycling through words. This week it was 'consistent'. I couldn't think of the word 'consistent'. I kept thinking it was 'coincident' or 'concentric' or 'constant'.” Such problems in executive function, memory, and processing speed are what many people complain about in the Long COVID support groups. Science validates their injuries. A picture is emerging from animal models showing how on-going inflammation of glial cells disrupts the electrical conduction highways in the brain's white matter that link to and support the neurons in gray matter. It's as if the bridges (white matter) linking different territories of the brain have been blown up and the land itself (nerves in the cerebral cortex and hippocampus) becomes scorched, leaving people with Long COVID plagued by thinking and memory deficits. ❂ 📖 (16 Feb 2023 ~ Stat) The haunting brain science of Long COVID ➤ © 2023 E. Wesley Ely / Stat.
by De Michele et al / Frontiers in Cardiovascular Medicine
•
18 January 2023
❦ ‘Acute ischemic stroke (AIS) is a fearful complication of Coronavirus Disease-2019 (COVID-19). SARS-CoV-2 infection seems to play a major role in endothelium activation and infarct volume extension during AIS.’ ❂ 📖 (10 Jan 2023 ~ Frontiers in Cardiovascular Medicine) SARS-CoV-2 infection predicts larger infarct volume in patients with acute ischemic stroke ➤ © 2023 Frontiers in Cardiovascular Medicine .
by Massimo et al / Brain
•
16 January 2023
❦ Strikingly, the [foetal brain] haemorrhages are predominantly found in the late first and early second trimester of gestation , a period of development in which the effect of the COVID-19 pandemic has not been thoroughly investigated. Specifically, the majority were between 12 and 14 PCW [post-conception week] , a critical window of human foetal brain development when the endothelial tight junctions increase to form the blood-brain barrier . Our observations of disrupted foetal cerebral vasculature are consistent with reports of damage to the microvasculature of the adult brain in SARS-CoV-2 infected patients . ❂ 📖 (16 Jan 2023 ~ Brain) Haemorrhage of human foetal cortex associated with SARS-CoV-2 infection ➤ © 2023 Massimo et al / Brain.
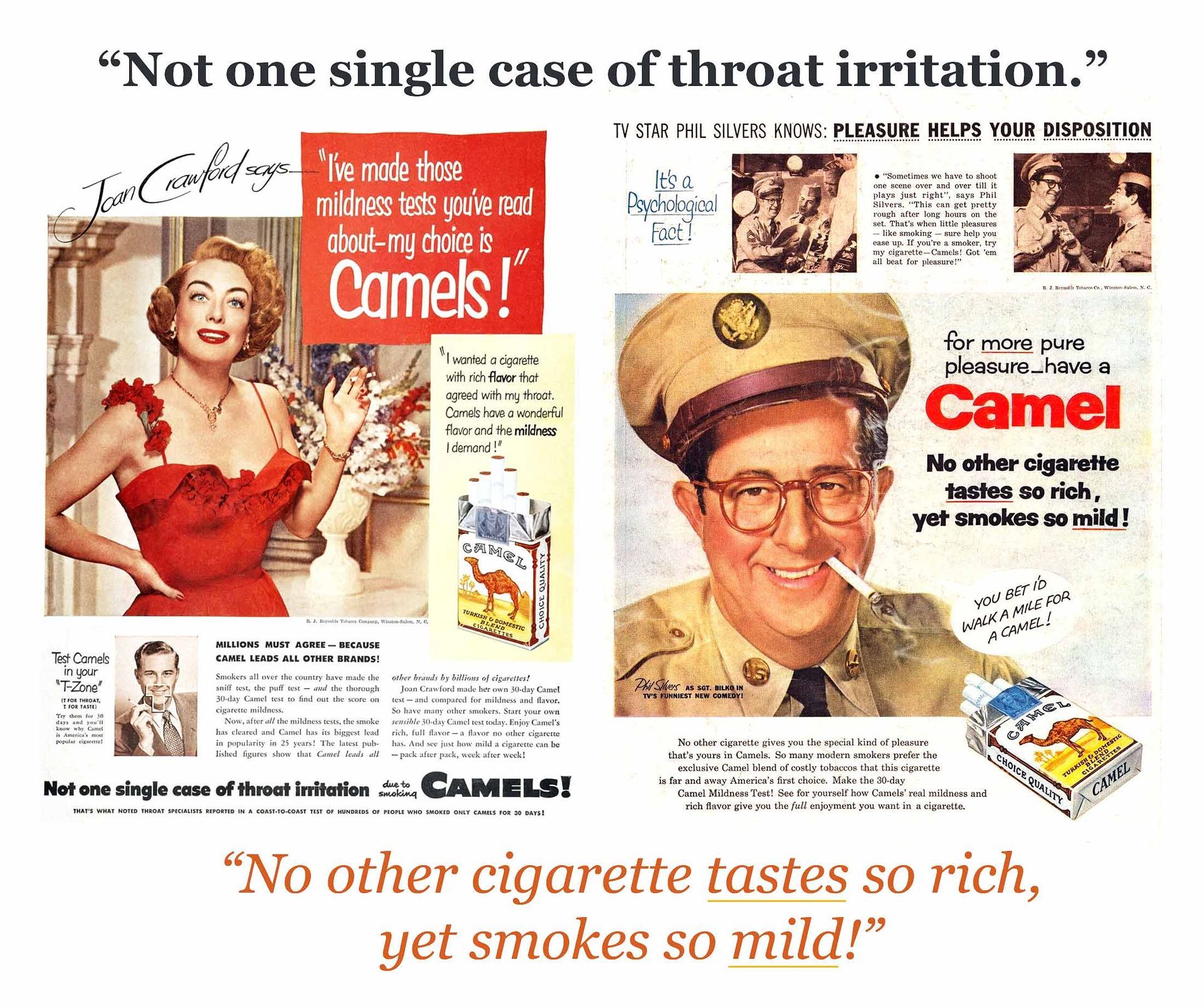
by Davis et al / Nature Reviews: Microbiology
•
13 January 2023
‘The narrative that COVID-19 had only respiratory sequelae led to a delayed realization of the neurological, cardiovascular and other multi-system impacts of COVID-19.’
by Wijeratne et al / University of Melbourne
•
6 January 2023
❦ Globally, millions of people have contracted COVID-19 over the past few years, and some have even caught the virus two or more times. Of more than 665 million cases worldwide, nearly one in two people with COVID-19 is at risk of developing Post-COVID-19 Neurological Syndrome (PCNS). Symptoms of Post-COVID-19 Neurological Syndrome (PCNS) mimic some of the symptoms we see after a stroke, and younger adults seem to be at particular risk. It’s worth noting that a link between brain health and Coronavirus infections has been known since 2006, so in this context the long-term impact of COVID-19 on the brain may arguably be the expectation rather than the exception. Nearly one in two people who have reportedly recovered from acute COVID-19 cite disabling fatigue – that is, fatigue lasting more than twelve weeks – coupled with a series of attention and cognitive deficits similar to persistent post-stroke neurological symptoms. We have already reported on the shared pathobiology between stroke and COVID-19 at a cellular level. So, it should not be surprising to see the long-term impact on the brain with a persistent inflammatory response (potentially due to viral persistence, immune dysregulation or autoimmunity). ❂ 📖 Related: (1 Jan 2023 ~ The Lancet) The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis ➤ 📖 Related: (7 Mar 2022 ~ Nature) SARS-CoV-2 is associated with changes in brain structure in UK Biobank ➤ 📖 Related: (12 Jan 2021 ~ Australian Journal of General Practice) COVID-19 and long-term neurological problems: Challenges ahead with Post-COVID-19 Neurological Syndrome ➤ 📖 Related: (1 Feb 2006 ~ Nature Reviews Microbiology) Coronavirus infection of the central nervous system: host-virus stand-off ➤ 📖 Related: (28 Jan 2021~ Frontiers in Neurology) COVID-19 Pathophysiology Predicts That Ischemic Stroke Occurrence Is an Expectation, Not an Exception - A Systematic Review ➤ ❂ 📖 (6 Jan 2023 ~ University of Melbourne) What we now know about long COVID and our brains ➤ © 2023 Wijeratne et al / University of Melbourne.
by LaRovere et al / JAMA: Neurology
•
1 January 2023
❦ ‘In 2021, SARS-CoV-2-related severe neurologic involvement in US hospitalized children and adolescents showed a potential increase in diagnoses of acute central nervous system infections / demyelination. In this case series of 2168 US patients younger than 21 years hospitalized for acute COVID-19 (34%) or multisystem inflammatory syndrome in children (66%), 476 (22%) had neurologic involvement. Of these, 42 (9%) had life-threatening conditions, with 23 (55%) having acute central nervous system (CNS) infections / demyelination; 18 of 42 (43%) died or had new neurologic deficits; and most vaccine-eligible patients were unvaccinated.’ ❂ 📖 (1 Jan 2023 ~ JAMA Network / Neurology) Changes in Distribution of Severe Neurologic Involvement in US Pediatric Inpatients With COVID-19 or Multisystem Inflammatory Syndrome in Children in 2021 vs 2020 ➤ 📖 Related: (5 Jan 2023 ~ Neurology Today) Nearly One-Fifth of Hospitalized Children and Adolescents with SARS-CoV-2 or MIS-C Have Persistent Neurologic Complications ➤ © 2023 LaRovere et al / JAMA: Neurology.
by Stein et al / Nature
•
22 December 2022
❦ ‘Others have previously reported SARS-CoV-2 RNA within the heart, lymph node, small intestine and adrenal gland. We replicate these findings and conclusively demonstrate that SARS-CoV-2 is capable of infecting and replicating within these and many other tissues, including brain. Our results show that although the highest burden of SARS-CoV-2 is in respiratory tissues, the virus can disseminate throughout the entire body.’ ❂ 📖 (14 Dec 2022 ~ Nature) SARS-CoV-2 infection and persistence in the human body and brain at autopsy ➤ © 2022 Stein et al / Nature.
by Mavrikaki et al / Nature: Aging
•
5 December 2022
❦ COVID-19 is an acute respiratory disease often accompanied by neurological sequelae. Individuals with previous severe COVID-19 exhibit a 10-year average drop in their global cognitive performance , mimicking accelerated aging . Complementary studies combining neuroimaging and cognitive screening implicate COVID-19-induced impairment of the frontal cortex, a critical area for cognitive function. Our findings indicate that COVID-19 is associated with molecular signatures of brain aging . ❂ 📖 (5 Dec 2022 ~ Nature Aging) Severe COVID-19 is associated with molecular signatures of aging in the human brain ➤ © 2023 Mavrikaki et al / Nature: Aging.
by Woodruff & Balmaceda / The University of Queensland, Australia
•
1 November 2022
❦ Research led by The University of Queensland has found COVID-19 activates the same inflammatory response in the brain as Parkinson’s disease. “We studied the effect of the virus on the brain’s immune cells, ‘microglia’ which are the key cells involved in the progression of brain diseases like Parkinson’s and Alzheimer’s,” Professor Woodruff said. “Our team grew human microglia in the laboratory and infected the cells with SARS-CoV-2, the virus that causes COVID-19. “We found the cells effectively became ‘angry’, activating the same pathway that Parkinson’s and Alzheimer’s proteins can activate in disease, the inflammasomes.” Dr Albornoz Balmaceda said triggering the inflammasome pathway sparked a ‘fire’ in the brain, which begins a chronic and sustained process of killing off neurons . “It’s kind of a silent killer , because you don’t see any outward symptoms for many years,” Dr Albornoz Balmaceda said. “It may explain why some people who’ve had COVID-19 are more vulnerable to developing neurological symptoms similar to Parkinson’s disease .” The researchers found the spike protein of the virus was enough to start the process and was further exacerbated when there were already proteins in the brain linked to Parkinson’s. “So if someone is already pre-disposed to Parkinson’s , having COVID-19 could be like pouring more fuel on that ‘fire’ in the brain,” Professor Woodruff said. “The same would apply for a predisposition for Alzheimer’s and other dementias that have been linked to inflammasomes.” ❂ 📖 (1 Nov 2022 ~ The University of Queensland, Australia) ‘ A silent killer’ – COVID-19 shown to trigger inflammation in the brain ➤ © 2022 Woodruff & Balmaceda / The University of Queensland, Australia.
by Xu, Xie & Al-Aly / Nature: Medicine
•
22 September 2022
❦ Our results show that in the postacute phase of COVID-19, there was increased risk of an array of incident neurologic sequelae including ischemic and hemorrhagic stroke , cognition and memory disorders , peripheral nervous system disorders , episodic disorders (for example, migraine and seizures ), extrapyramidal and movement disorders , mental health disorders , musculoskeletal disorders , sensory disorders , Guillain-Barré syndrome , and encephalitis or encephalopathy . ❂ 📖 Related: (22 Sep 2022 ~ Washington University School of Medicine in St. Louis) COVID-19 infections increase risk of long-term brain problems ➤ Those who have been infected with the [SARS-CoV-2] virus are at increased risk of developing a range of neurological conditions in the first year after the infection. Such complications include strokes, cognitive and memory problems, depression, anxiety and migraine headaches. Additionally, the post-COVID brain is associated with movement disorders, from tremors and involuntary muscle contractions to epileptic seizures, hearing and vision abnormalities, and balance and coordination difficulties as well as other symptoms similar to what is experienced with Parkinson’s disease. ❂ 📖 (22 Sep 2022 ~ Nature Medicine) Long-term neurologic outcomes of COVID-19 ➤ © 2022 Xu, Xie & Al-Aly / Nature: Medicine.
by Davis et al / Journal of Alzheimer’s Disease
•
13 September 2022
‘Older people who were infected with COVID-19 show a substantially higher risk – as much as 50% to 80% higher – of developing Alzheimer’s disease within a year. And the highest risk was observed in women at least 85 years old.’
by Dr. Noor Bari, Emergency Medicine
•
21 July 2022
❦ “So, we want to “live with the virus”. Is there any evidence of this occurring successfully anywhere? Yes! In bats... and it has taken 64 million years of evolution to get there. To “live with the virus”, bats have better host defences – they don’t overdo inflammation, and they can get rid of toxic compounds and deal with reactive oxygen species much better than humans. They literally live with the virus .
by Lopez-Leon et al / Nature
•
23 June 2022
❦ ‘The prevalence of Long COVID in children and adolescents was 25.24% . The five most prevalent clinical manifestations were mood symptoms (16.50%), fatigue (9.66%), sleep disorders (8.42%), headache (7.84%), and respiratory symptoms (7.62%). Interestingly, many of the symptoms identified in these meta-analyses associated to Long COVID, such as mood, fatigue, sleep disorders, orthostatic intolerance, decreased concentration, confusion, memory loss, balance problems, exercise intolerance, hyperhidrosis, blurred vision, body temperature dysregulation, dysfunction on heart, rate variability and palpitations, constipation or diarrhea, and dysphagia, are commonly present in dysautonomia .’ ❂ 📖 (23 Jun 2022 ~ Nature Scientific Reports) Long COVID in children and adolescents: a systematic review and meta-analyses ➤ © 2022 Lopez-Leon et al / Nature.
by Sumeet Kulkarni / LA Times
•
10 June 2022
❦ ‘Babies whose mothers were infected with the coronavirus during pregnancy may face a higher risk of brain development disorders such as autism and bipolar disorder, a new study that examined more than 7,500 births suggests. Other viruses, such as influenza and measles, are thought to make babies more vulnerable to conditions such as autism, schizophrenia and depression if they are exposed in utero. After the researchers accounted for other factors that could affect a child’s risk for a neurodevelopmental issue — such as pre-term births, the mother’s age and the baby’s gender — they calculated that babies with prenatal exposure to SARS-CoV-2 were 86% more likely to be diagnosed in their first year compared with babies who weren’t exposed before they were born. “Unfortunately, it is very possible that asymptomatic or mild infections might also be linked to neurodevelopmental disorders in the child.” The medical advice for pregnant women remains unchanged. “This should be another wake-up call for pregnant women to get vaccinated, and boosted, and stay masked and take as many precautions as they can.” ❂ 📖 (10 Jun 2022 ~ LA Times) Coronavirus infection during pregnancy linked to brain development problems in babies ➤ 📖 (9 June 2022 ~ JAMA Network Open) Neurodevelopmental Outcomes at 1 Year in Infants of Mothers Who Tested Positive for SARS-CoV-2 During Pregnancy ➤ © 2022 Sumeet Kulkarni / LA Times
by Edlow et al / JAMA: Pediatrics
•
9 June 2022
❦ ‘In this analysis of 222 offspring of mothers infected with SARS-CoV-2, compared with the offspring of 7550 mothers in the control group (not infected) delivered during the same period, we observed neurodevelopmental diagnoses to be significantly more common among exposed offspring, particularly those exposed to third-trimester maternal infection . The majority of these diagnoses reflected developmental disorders of motor function or speech and language .’ ❂ 📖 (9 Jun 2022 ~ JAMA: Pediatrics) Neurodevelopmental Outcomes at 1 Year in Infants of Mothers Who Tested Positive for SARS-CoV-2 During Pregnancy ➤ © 2022 Edlow et al / JAMA: Pediatrics.
by Buonsenso et al / Future Microbiology
•
1 April 2022
❦ ‘The authors performed a survey in children suffering from persistent symptoms since initial infection. A total of 510 children infected between January 2020 and January 2021 were included. Symptoms such as fatigue, headache, muscle and joint pain, rashes and heart palpitations and issues such as lack of concentration and short-term memory problems were particularly frequent and confirm previous observations, suggesting that they may characterize this condition.’ ❂ 📖 (1 Apr 2022 ~ Future Microbiology) Clinical characteristics, activity levels and mental health problems in children with long coronavirus disease: a survey of 510 children ➤ © 2022 Buonsenso et al / Future Microbiology.
by RTHM
•
24 February 2022
❦ Headaches are one of the most common non-respiratory symptoms associated with SARS-CoV-2 and COVID-19. In fact, for most, a headache was the first initial symptom of the infection. For many, the headaches resolve after recovery from the acute infection. However, headaches are also one of the most common symptoms experienced by those with Long COVID. These migraine-like headaches can often last for weeks or even months, leaving many unable to perform routine daily activities. ❦ Headaches are a main symptom of acute COVID-19 While originally considered a respiratory virus, respiratory symptoms are not always the first indicator of a COVID infection. For example, for many, the first symptom is the loss of taste and/or smell ('anosmia'). Researchers believe that this may occur due to the virus entering the nasal cavity and crossing over into the brain. In this same way, many people often experience a severe headache in addition to the anosmia. ❦ How is a COVID headache different to a migraine? Many describe a COVID headache as crushing pain spread throughout the skull that can cause a pulsing or pressing pain. This pain typically worsens with physical activity or movement of the head. For this reason, many often refer to it as a migraine. However, a migraine is considered a primary headache. A COVID headache, on the other hand, is considered a secondary headache due to an underlying condition – in this case, the SARS-CoV-2 viral infection. While both types of headaches produce moderate to severe pain intensity, there are some differences between a traditional migraine and a COVID headache. COVID headache vs. migraine: ❦ Missing common additional symptoms ~ Migraines often come with nausea, vomiting, and a sensitivity to light and sound. In addition, many often experience an aura before headache onset. None of these symptoms typically accompany a COVID headache. ❦ Different pain ~ In many cases, migraines occur unilaterally, or on one side. COVID headaches are typically bilateral and affect the entire head. ❦ Do not respond to medication ~ If you have a history of migraines and take prescribed medication, you may find the COVID headache does not respond. In fact, a COVID headache is unlikely to respond to traditional headache medications in general, including over-the-counter pain medications such as acetaminophen or ibuprofen. Headaches continue with Long COVID Lingering headaches are not uncommon after viral infections, so it was no surprise to see headaches become a symptom associated with Long COVID. However, the persistence and severity of headaches with Long COVID has been different than with previous viral infections. While many of these headaches do improve on their own over time, many people continue to struggle with severe headaches that can last for weeks or months. In many cases, people will have a baseline headache that gets worse from time to time, along with other Long COVID symptoms. What is causing COVID headaches? [At the time of writing (24 Feb 2022)] the exact cause of these COVID headaches is unknown. However, researchers and clinicians have some theories. 1. Researchers propose that the trigeminal nerve endings in the nasal cavity may sustain direct viral damage that activates the trigeminovascular system, resulting in headaches, as well as other cognitive symptoms. 2. Studies are showing that many COVID patients are experiencing unusual microclots in their blood after recovering from the acute infection. These microclots can prevent adequate oxygen transportation throughout the body and contribute to Long COVID symptoms, including headaches. 3. Neurological damage has been seen in many COVID and Long COVID patients, but the exact cause of this damage is still unknown. Some theories believe that the virus may be able to cause direct damage to the brain by entering through the olfactory bulb or through the bloodstream or nerve endings. In addition, as your body fights the virus, your immune system often goes into overdrive, creating autoantibodies that attack healthy cells within the body and cause damage. 4. Jaw or dental concerns. ❂ 📖 Related: (19 July 2021 ~ Nature / Scientific Reports) Frequency and phenotype of headache in Covid-19: a study of 2194 patients ➤ 📖 Related: (15 May 2020 ~ Headache: The Journal of Head and Face Pain) COVID-19 is a Real Headache! ➤ 📖 Related: (9 May 2022 ~ Preprint) Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID / Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms ➤ ❂ 📖 (24 Feb 2022 ~ RTHM) Long COVID: Migraines and Headaches ➤ © 2022 RTHM.
by Parkinson’s Foundation
•
22 February 2022
❦ It has long been suspected by scientists that the flu (influenza) might play a role in developing Parkinson’s disease (PD) later in life. Compared to those who were not diagnosed with the flu, there was a 90% higher risk of PD for those who had the flu 15 or more years earlier. Inflammation is clearly a factor in PD – and influenza is known to trigger an extreme inflammatory response in the body. In light of the COVID-19 pandemic, and its known neurological consequences such as brain fog and loss of smell, continued robust research into how inflammation impacts the brain is warranted. ❂ 📖 (22 Feb 2022 ~ Parkinson's Foundation) The Flu Factor: Is There a Link to Parkinson's? ➤ © 2022 Parkinson’s Foundation.
by Shook et al / Trends in Molecular Medicine
•
13 February 2022
❦ SARS-CoV-2 infection in pregnancy is known to confer a risk of increased morbidity and mortality for the mother. Placental and fetal infection with SARS-CoV-2 have been rare to date; SARS-CoV-2 infection in pregnancy appears most likely to impact fetal brain development via maternal and placental immune activation. Maternal and placental immune activation may impact the placenta and developing fetal brain via induction of immune activation and proinflammatory cytokine production, dysregulation of serotonin/other neurotransmitter signaling, and increased oxidative stress. ❂ 📖 (13 Feb 2022 ~ Trends in Molecular Medicine) COVID-19 in pregnancy: implications for fetal brain development ➤ © 2022 Shook et al / Trends in Molecular Medicine.
by Pyne and Brickman / Neurodegenerative Diseases
•
28 July 2021
‘SARS-CoV-2 infection initiates a disease progression that has the potential to promote cognitive decline and exacerbate pre-existing dementia.’
by MedicalXpress
•
22 June 2021
❦ The brains of people who died from COVID-19 were remarkably similar to the brains of people who die from neurodegenerative diseases such as Alzheimer’s and Parkinson’s , showing inflammation and disrupted circuitry . — “The brains of patients who died from severe COVID-19 showed profound molecular markers of inflammation , even though those patients didn’t have any reported clinical signs of neurological impairment,” said study co-senior author Tony Wyss-Coray, a professor of neurology and neurological sciences at Stanford University. His team analyzed brain tissue from eight people who died of COVID-19 and 14 people who died of other causes. About one-third of hospitalized COVID-19 patients report neurological symptoms such as fuzzy thinking , forgetfulness , difficulty concentrating and depression , Wyss-Coray noted. These problems can persist as part of what’s called Long COVID, a lingering condition that sometimes affects patients after they recover from the original infection. ❂ 📖 (21 Jun 2021 ~ Nature) Dysregulation of brain and choroid plexus cell types in severe COVID-19 ➤ 📖 (22 Jun 2021 ~ MedicalXpress) Autopsy study shows how COVID harms the brain ➤ © 2021 MedicalXpress.
More... PASC (‘Long Covid’)
by C19.Life... et al
•
21 November 2025
‘Although COVID-19 was originally considered a respiratory illness, it is now well established that SARS-CoV-2 infection can have far-reaching impacts on the nervous system. Common neurological symptoms in Long COVID [PASC] include new-onset cognitive difficulties, dysautonomia, fatigue, and peripheral neuropathy.’ from ‘Neuroimmune pathophysiology of long COVID’ by Moen et al / Psychiatry and Clinical Neurosciences (2025).
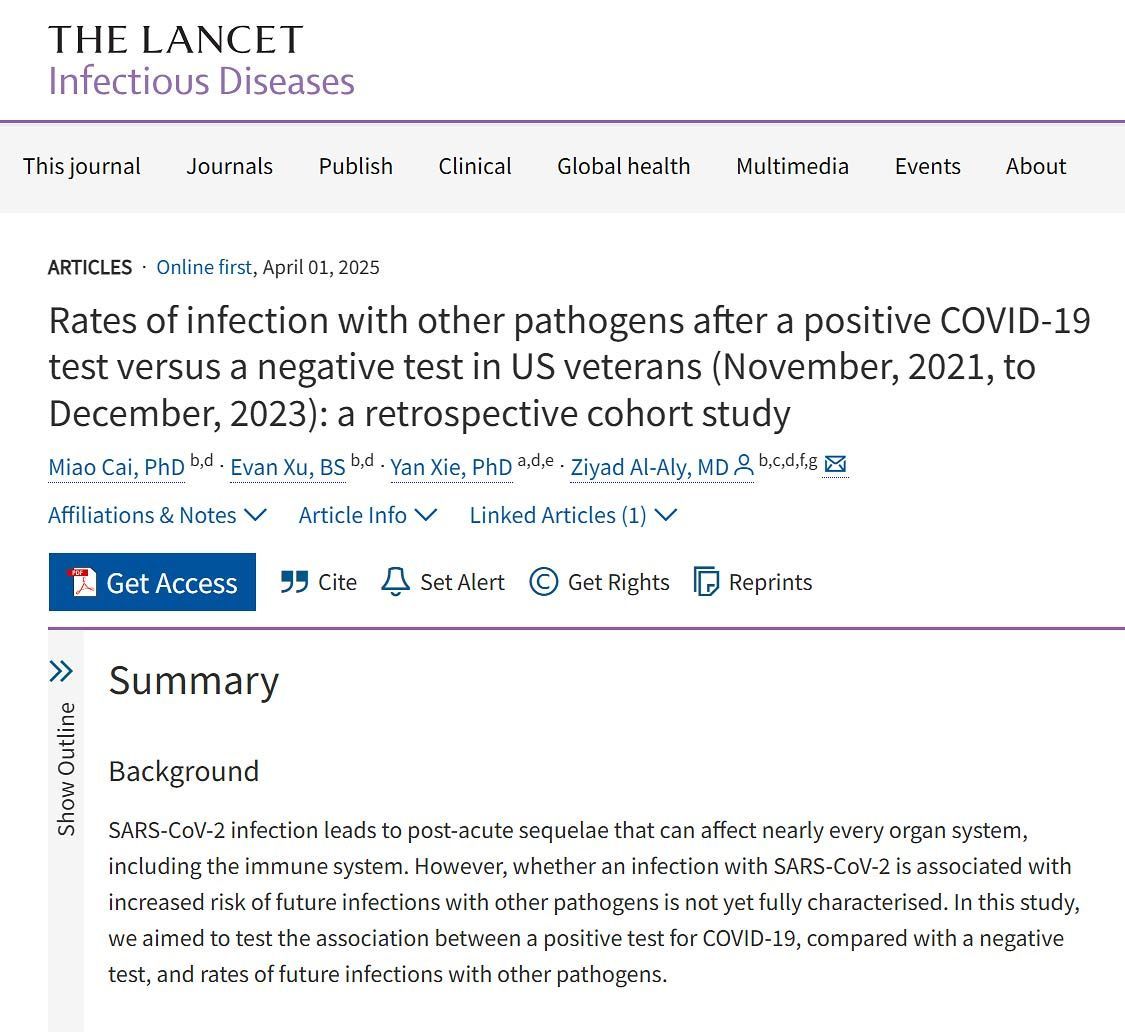
by CIDRAP ❂ Cai et al / The Lancet: Infectious Diseases
•
2 April 2025
‘These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens.’
by David Putrino ❂ Sonya Buyting ~ Radio-Canada / Canadian Broadcasting Corporation
•
20 March 2025
CBC Radio-Canada interview with long COVID [PASC] researcher David Putrino from the Icahn School of Medicine at Mount Sinai in New York.
by Jason Gale / Bloomberg UK
•
3 March 2025
‘For patients already battling Alzheimer’s disease, studies indicate that Covid can exacerbate brain inflammation, damage immune cells, and accelerate the disease. Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection. Mild Covid cases in younger adults have also been linked to brain issues affecting memory and thinking. ’
by C19.Life... et al
•
28 February 2025
‘But even people who had not been hospitalized had increased risks of many conditions, ranging from an 8% increase in the rate of heart attacks to a 247% increase in the rate of heart inflammation.’ Nature (2 Aug 2022) ‘Either symptomatic or asymptomatic SARS-CoV-2 infection is associated with increased risk of late cardiovascular outcomes and has causal effect on all-cause mortality in a late post-COVID-19 period.’ The American Journal of Cardiology (15 Sep 2023)
by Huang et al / BMC Medicine
•
6 February 2025
‘The proportions of PACS [PASC/Long Covid] patients experiencing chest pain, palpitation, and hypertension as sequelae were 22%, 18%, and 19% respectively.’
by News Medical Life Sciences ❂ Duff et al / Nature Medicine
•
2 February 2025
‘Scientists discover that even mild COVID-19 can alter brain proteins linked to Alzheimer’s disease, potentially increasing dementia risk. COVID-19-positive individuals exhibited lower cognitive test performance compared to controls – equivalent to almost two years of age-related cognitive decline. ’
by R. Peter et al / PLOS Medicine
•
23 January 2025
‘The predominant symptoms, often clustering together, remain fatigue, cognitive disturbance and chest symptoms, including breathlessness, with sleep disorder and anxiety as additional complaints. Many patients with persistent PCS [PASC/‘Long Covid’] show impaired executive functioning, reduced cognitive processing speed and reduced physical exercise capacity.’
by C19.Life
•
16 November 2024
❦ On that 700-day cough... It’s a new thing, but it’s only reserved for inside supermarkets and offices. And pharmacies and hospitals and care homes. Oh, and your living-room. But apart from that, it’s not exactly a deal-breaker. I mean, c’mon. They put up with way worse in the 1900s.
by Porter et al / The Lancet: Regional Health (Americas)
•
23 October 2024
❦ ‘In this population of healthy young adult US Marines with mostly either asymptomatic or mild acute COVID-19, one fourth reported physical , cognitive , or psychiatric long-term sequelae of infection. The Marines affected with PASC [Post-Acute Sequelae of COVID-19 / Post-COVID-19 Complications / ‘Long Covid’] showed evidence of long-term decrease in functional performance suggesting that SARS-CoV-2 infection may negatively affect health for a significant proportion of young adults .’ ❂ ‘Among the 899 participants, 88.8% had a SARS-CoV-2 infection. Almost a quarter (24.7%) of these individuals had at least one COVID-19 symptom that lasted for at least 4 weeks meeting the a priori definition of PASC established for this study. Among those with PASC, 10 had no acute SARS-CoV-2 symptoms after PCR-confirmed infection suggesting that PASC can occur among asymptomatic individuals. Many participants reported that lingering symptoms impaired their productivity at work, caused them to miss work, and/or limited their ability to perform normal duty/activities. Marines with PASC had significantly decreased physical fitness test scores up to approximately one year post-infection with a three-mile run time that averaged in the 65th percentile of the reference cohort. [ PASC was associated with a significantly increased 3-mile run time on the standard Marine fitness test. PASC participants ran 25.1 seconds slower than a pre-pandemic reference cohort composed of 22,612 Marine recruits from 2016 to 2019. A three-mile run evaluates aerobic exercise , overhead lifting of an ammunition can and pull-ups evaluate strength , and shooting a rifle evaluates fine-motor skills .] Scores for events evaluating upper body (pull-ups, crunches, and ammo-can lift) were not significantly reduced by PASC; however, overall physical fitness scores were reduced. ‘The poorer run times and overall scores among PASC participants are indicative of on-going functional effects.’ Standardized health-based assessments for somatization, depression, and anxiety further highlighted the detrimental health effects of PASC. Almost 10% of participants with PASC had PHQ-8 scores ≥10. Increased somatization * has been associated with increased stress, depression, and problems with emotions. * [ Somatization / Somatisation = Medical symptoms caused by psychological stress.] Additionally, PASC participants had higher GAD-7 scores suggesting increased anxiety in a population with unique inherent occupational stressors associated with higher rates of anxiety, depression, and post-traumatic stress disorder. ‘Increased severity of anxiety among those with PASC, combined with greater rates of mental health disorders in general, could portend an ominous combination and should be closely followed.’ Like others, we identified cardiopulmonary symptoms as some of the most prevalent. The high prevalence of symptoms like shortness of breath, difficulty breathing, cough, and fatigue is particularly notable when combined with decreased objective measures of aerobic performance such as running. These results suggest pathology in the cardiopulmonary system. In contrast we observed no reduction in scores assessing strength and marksmanship suggesting the lack of detectable pathology in the neuro-musculoskeletal system. We have previously found in this same cohort that SARS-CoV-2 infection causes prolonged dysregulation of immune cell epigenetic patterns like auto-immune diseases. Based on the reported PASC symptoms, the potential current and future public health implications in this population could be substantial. ‘Chronic health complications from PASC, especially in a young and previously healthy population with a long life expectancy, could decrease work productivity and increase healthcare costs.’ Significant changes in the Years-of-Life lived with a disability can disproportionally increase disability-adjusted life-years, and should be considered when allocating resources and designing policy.’ ❂ 📖 (23 Oct 2024 ~ The Lancet: Regional Health/America) Clinical and functional assessment of SARS-CoV-2 sequelae among young marines – a panel study ➤ © 2024 The Lancet .
by Dempsey et al / BMJ Journals ~ Occupational and Environmental Medicine
•
8 October 2024
‘This study included 5248 healthcare workers. While 33.6% reported prolonged COVID-19 symptoms consistent with PCS, only 7.4% reported a formal diagnosis of PCS. Fatigue, difficulty concentrating, insomnia, and anxiety or depression were the most common PCS [Post-COVID-19 Syndrome] symptoms. Baseline risk factors for reporting PCS included screening for common mental disorders, direct contact with COVID-19 patients, pre-existing respiratory illnesses, female sex and older age.’
by Al-Aly & Topol / Science
•
22 February 2024
‘Reinfection, which is now the dominant type of SARS-CoV-2 infection, is not inconsequential; it can trigger de novo Long Covid or exacerbate its severity. Each reinfection contributes additional risk of Long Covid: cumulatively, two infections yield a higher risk of Long Covid than one infection, and three infections yield a higher risk than two infections.’
by Greene et al / Nature: Neuroscience [Commentary by Danielle Beckman]
•
22 February 2024
❦ “This study confirms everything that I have seen in the microscope over the last few years. The authors of the study use a technique called dynamic contrast-enhanced magnetic resonance imaging ( DCE-MRI ), an imaging technique that can measure the density , integrity , and leakiness of tissue vasculature. Comparing all individuals with previous COVID infection to unaffected controls revealed decreased general brain volume in patients with ‘brain fog’ – along with significantly reduced cerebral white matter volume in both hemispheres in the recovered and ‘brain fog’ cohorts . Covid-19 induces brain-volume loss and leaky blood-brain barrier in some patients. How can this be more clear?” © 2024 Dr. Danielle Beckman, Neuroscientist (PhD Biological Chemistry) ➲ ❂ 📖 (22 Feb 2024 ~ Nature: Neuroscience) Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment ➤ ‘ Our data suggest that sustained systemic inflammation and persistent localized blood-brain barrier (BBB) dysfunction is a key feature of long COVID-associated brain fog. Patients with long COVID had elevated levels of IL-8, GFAP and TGFβ, with TGFβ specifically increased in the cohort with brain fog. GFAP is a robust marker of cerebrovascular damage and is elevated after repetitive head trauma, reflecting BBB disruption, as seen in contact sport athletes and in individuals with self-reported neurological symptoms in long COVID. Interestingly, TGFβ was strongly associated with BBB disruption and structural brain changes. ’ [Layperson overview] 📖 (February 2024 ~ Genetic Engineering and Biotechnology News) Leaky Blood Vessels in the Brain Linked to Brain Fog in Long COVID Patients ➤ [Related] 📖 (7 Feb 2022 ~ Nature: Cardiovascular Research) Blood–brain barrier link to human cognitive impairment and Alzheimer’s disease ➤ ❂
by Meng et al / The Lancet: eClinical Medicine
•
17 February 2024
❦ ‘The occurrences of respiratory disorders among patients who survived for 30 days after the COVID-19 diagnosis continued to rise consistently, including asthma , bronchiectasis , COPD , ILD , PVD * , and lung cancer . * COPD = Chronic obstructive pulmonary disease . ILD = Interstitial lung disease . PVD = Peripheral vascular disease . With the severity of the acute phase of COVID-19, the risk of all respiratory diseases increases progressively. Besides, during the 24-months follow-up, we observed an increasing trend in the risks of asthma and bronchiectasis over time, which indicates that long-term monitoring and meticulous follow-up of these patients is essential. These findings contribute to a more complete understanding of the impact of COVID-19 on the respiratory system and highlight the importance of prevention and early intervention of these respiratory sequelae of COVID-19. In this study, several key findings have been further identified. Firstly, our research demonstrates a significant association between COVID-19 and an increased long-term risk of developing various respiratory diseases. Secondly, we found that the risk of respiratory disease increases with severity in patients with COVID-19, indicating that it is necessary to pay attention to respiratory COVID-19 sequelae in patients, especially those hospitalized during the acute stage of infection. This is consistent with the findings of Lam et al., who found that the risk of some respiratory diseases (including chronic pulmonary disease, acute respiratory distress syndrome and ILD) increased with the severity of COVID-19. Notably, however, our study found that asthma and COPD remained evident even in the non-hospitalized population. This emphasizes that even in cases of mild COVID-19, the healthcare system should remain vigilant. Thirdly, we investigated differences in risk across time periods, as well as the long-term effects of COVID-19 on respiratory disease. During the 2-years follow-up period, the risks of COPD, ILD, PVD and lung cancer decreased, while risks of asthma and bronchiectasis increased. Fourthly, our study showed a significant increase of the long-term risk of developing asthma, COPD, ILD, and lung cancer diseases among individuals who suffered SARS-CoV-2 reinfection. This finding emphasizes the importance of preventing reinfection of COVID-19 in order to protect public health and reduce the potential burden of SARS-CoV-2 reinfection. Interestingly, vaccination appears to have a potentially worsening effect on asthma morbidity compared with other outcomes. This observation aligns with some previous studies that have suggested a possible induction of asthma onset or exacerbation by COVID-19 vaccination. It suggests that more care may be necessary for patients with asthma on taking the COVID vaccines. The underlying mechanisms associated with COVID and respiratory outcomes are not fully understood, but several hypotheses have been proposed. First, SARS-CoV-2 can persist in tissues (including the respiratory tract), as well as the circulating system for an extended period of time after the initial infection. This prolonged presence of the virus could directly contribute to long-term damage of the respiratory tissues, consequently leading to the development of various respiratory diseases. Second, it has been observed that SARS-CoV-2 infection can lead to prolonged immunological dysfunctions, including highly activated innate immune cells, a deficiency in naive T and B cells, and increased expression of interferons and other pro-inflammatory cytokines. These immune system abnormalities are closely associated with common chronic respiratory diseases – asthma, bronchiectasis, COPD, as well as the development of lung cancer. Next, SARS-CoV-2 itself has been shown to drive cross-reactive antibody responses, and a range of autoantibodies were found in patients with COVID-19. In conclusion, our research adds to the existing knowledge regarding the effects of COVID-19 on the respiratory system. Specifically, it shows that the risk of respiratory illness increases with the severity of infection and reinfection. Our findings emphasize the importance of providing extended care and attention to patients previously infected with SARS-CoV-2.’ ❂ 📖 (17 Feb 2024 ~ The Lancet: eClinical Medicine) Long-term risks of respiratory diseases in patients infected with SARS-CoV-2: a longitudinal, population-based cohort study ➤ © 2024 The Lancet: eClinical Medicine .
by Henry Madison
•
9 February 2024
❦ “Chronic disease is like the perfect medical crime. The cause is usually long gone by the time the disease manifests, and nobody links the two until it’s much too late for most.” ❂ © 2024 Henry Madison . ➲
by Dr. David Joffe PhD / FRACP (Respiratory Physician)
•
27 January 2024
❦ “It’s really not in the interest of the virus to kill us quickly. That’s why it has mutated to immune escape. That way it enters silently, and then eats you slowly whilst you’re still a spreading vector. Refrigerator trucks are long gone. That’s all the political class wanted. The unseen costs of CVD [cardiovascular disease] , DM [diabetes mellitus] , and both dementia and Parkinson’s Disease are the train coming down the tunnel. The economists are catching up. The actuaries are already there. Politicians and most people? Not yet...” ❂ © 2024 Dr. David Joffe PhD / FRACP (Respiratory Physician) ➲
by Scardua-Silva et al / Nature: Scientific Reports
•
19 January 2024
❦ ‘Although some studies have shown neuroimaging and neuropsychological alterations in post-COVID-19 patients, fewer combined neuroimaging and neuropsychology evaluations of individuals who presented a mild acute infection. Here we investigated cognitive dysfunction and brain changes in a group of mildly infected individuals. We conducted a cross-sectional study of 97 consecutive subjects ( median age of 41 years ) without current or history of psychiatric symptoms (including anxiety and depression) after a mild infection , with a median of 79 days (and mean of 97 days ) after diagnosis of COVID-19. We performed semi-structured interviews, neurological examinations, 3T-MRI scans, and neuropsychological assessments. The patients reported memory loss ( 36% ), fatigue ( 31% ) and headache ( 29% ). The quantitative analyses confirmed symptoms of fatigue ( 83% of participants), excessive somnolence ( 35% ), impaired phonemic verbal fluency ( 21% ), impaired verbal categorical fluency ( 13% ) and impaired logical memory immediate recall ( 16% ). Our group… presented higher rates of impairments in processing speed ( 11.7% in FDT- Reading and 10% in FDT- Counting ). The white matter (WM) analyses with DTI * revealed higher axial diffusivity values in post-infected patients compared to controls. * Diffusion tensor imaging tractography , or DTI tractography, is an MRI (magnetic resonance imaging) technique most commonly used to provide imaging of the brain. Our results suggest persistent cognitive impairment and subtle white matter abnormalities in individuals mildly infected , without anxiety or depression symptoms. One intriguing fact is that we observed a high proportion of low average performance in our sample of patients (which has a high average level of education ), including immediate and late verbal episodic memory, phonological and semantic verbal fluency, immediate visuospatial episodic memory, processing speed, and inhibitory control . Although most subjects did not present significant impaired scores compared with the normative data, we speculate that the low average performance affecting different domains may result in a negative impact in everyday life , especially in individuals with high levels of education and cognitive demands .’ ❂ ❦ Note how these findings might negatively affect daily activities that demand sustained cognitive attention and fast reaction times – such as driving a car or motorbike, or piloting a plane. Consider air-traffic control. Consider the impact on healthcare workers whose occupations combine long periods of intense concentration with a need for critical precision. ❂ 📖 (19 Jan 2024 ~ Nature: Scientific Reports) Microstructural brain abnormalities, fatigue, and cognitive dysfunction after mild COVID-19 ➤ © 2024 Nature .
by Harris et al / Current Osteoporosis Reports
•
18 January 2024
‘ Clinical evidence suggests that SARS-CoV-2 may lead to hypocalcemia, altered bone turnover markers, and a high prevalence of vertebral fractures. ’
by Wolfram Ruf / Science
•
18 January 2024
❦ ‘Acute infections with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cause a respiratory illness that can be associated with systemic immune cell activation and inflammation , widespread multi-organ dysfunction , and thrombosis . Not everyone fully recovers from COVID-19, leading to Long Covid, the treatment of which is a major unmet clinical need. Long Covid can affect people of all ages , follows severe as well as mild disease , and involves multiple organs . Patients with Long Covid display signs of immune dysfunction and exhaustion , persistent immune cell activation , and autoimmune antibody production , which are also pathological features of acute COVID-19. The complement system is crucial for innate immune defense by effecting lytic destruction of invading micro-organisms, but when uncontrolled, it causes cell and vascular damage . The complement cascade is activated by antigen–antibody complexes in the classical pathways or in the lectin pathway by multimeric proteins (lectins) that recognize specific carbohydrate structures, which are also found on the SARS-CoV-2 spike protein that facilitates host cell entry. Both pathways may contribute to the pronounced complement activation in acute COVID-19. Long Covid symptoms include a postexertional exhaustion reminiscent of other post-viral illnesses , such as myalgic encephalomyelitis ( ME ) – chronic fatigue syndrome ( MECFS ) with suspected latent viral reactivation . Antibody titer changes in Long Covid patients indicate an association of fatigue with reactivation of latent Epstein-Barr virus ( EBV ) infections , and Cervia-Hasler et al found that the severity of Long Covid symptoms is associated with cytomegalovirus ( CMV ) reactivation . A better understanding of the connections between viral reactivation, persistent interferon signaling, and autoimmune pathologies promises to yield new insights into the thromboinflammation associated with Long Covid. Although therapeutic interventions with coagulation and complement inhibitors in acute COVID-19 produced mixed results, the pathological features specific for Long Covid suggest potential interventions for clinical testing. Microclots are also observed in ME-CFS patients , indicating crucial interactions between complement, vWF, and coagulation-mediated fibrin formation in post-viral syndromes. A better definition of these interactions in preclinical and clinical settings will be crucial for the translation of new therapeutic concepts in chronic thromboinflammatory diseases .’ ❂ 📖 (18 Jan 2024 ~ Science) Immune damage in Long Covid ➤ © 2024 Wolfram Ruf / Science .
by Michael Merschel / American Heart Association
•
16 January 2024
“I would argue that COVID-19 is not a disease of the lungs at all. It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system.”
by Shajahan et al / Frontiers in Aging Neuroscience
•
8 January 2024
‘[COVID-19’s] ability to invade the central nervous system through the hematogenous and neural routes, besides attacking the respiratory system, has the potential to worsen cognitive decline in Alzheimer’s disease patients. The severity of this issue must be highlighted.’
by Appelman et al / Nature Communications
•
4 January 2024
Post-exertional malaise (PEM) is a marked physical or mental fatigue and deterioration of symptoms occurring after physical , cognitive , social or emotional exertion that would have been tolerated previously. Symptoms typically worsen 12 to 48 hours after such activities , and can last for days , weeks or months , making it difficult to manage or predict. PEM is a hallmark symptom of myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS), and is commonly reported by people with Post-COVID-19 Syndrome (PCS/‘Long Covid’). PEM can be mitigated by activity management , or ‘ pacing ’.
by Carolyn Barber / Fortune & Outbreak Updates
•
14 December 2023
❦ ‘Al-Aly’s study undertook a comparative analysis of 94 pre-specified health outcomes and found that over 18 months of follow-up, COVID was associated with a “ significantly increased risk ” for 64 of them, or nearly 70% . The disease’s enhanced risk list includes everything from cardiac arrest , stroke , chronic kidney disease , and cognitive impairment to mental health and fatigue , characteristics often associated with long COVID. By comparison, the seasonal flu was associated with increased risk in only 6 of the 94 conditions specified. Further, while COVID increased the risks for almost all the organ systems studied, the flu heightened risk primarily for the pulmonary ( lung ) system . Those findings, Al-Aly says, suggest that “ COVID is really a multi-systemic disease , and flu is more a respiratory virus ”.’ ❂ 📖 (14 Dec 2023 ~ Fortune) COVID-19 v. Flu: A ‘much more serious threat,’ new study into long-term risks concludes ➤ 📖 (14 Dec 2023 ~ The Lancet) Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study ➤ © 2023 Carolyn Barber / Fortune .
by Bland et al / Occupational Medicine
•
11 December 2023
❦ ‘As a consequence of their occupation, doctors and other healthcare workers were at higher risk of contracting coronavirus disease 2019 (COVID-19), and more likely to experience severe disease compared to the general population. Post-acute COVID (Long COVID) in UK doctors is a substantial burden. Insufficient respiratory protection could have contributed to occupational disease, with COVID-19 being contracted in the workplace , and resultant post-COVID complications. Although it may be too late to address the perceived determinants of inadequate protection for those already suffering with Long COVID, more investment is needed in rehabilitation and support of those afflicted .’ ❂ 📖 (11 Dec 2023 ~ Occupational Medicine) Post-acute COVID-19 complications in UK doctors: results of a cross-sectional survey ➤
by Pearson-Stuttard et al / The Lancet (Regional Health Europe)
•
1 December 2023
❦ 'For middle-aged adults ( 50–64 ) in this period [June 2022 – June 2023 ], the relative excess for almost all causes of death examined was higher than that seen for all ages .' ➲ ‘Since July 2020, the Office for Health Improvement and Disparities (OHID) has published estimates of excess mortality. In the period from week ending 3rd June 2022 to 30th June 2023 , excess deaths for all causes were relatively greatest for 50–64 year olds ( 15% higher than expected ), compared with 11% higher for 25–49 and < 25 year olds , and about 9% higher for over 65 year old groups. Several causes, including cardiovascular diseases , show a relative excess greater than that seen in deaths from all-causes ( 9% ) over the same period (week ending 3rd June 2022–30th June 2023), namely: all cardiovascular diseases ( 12% ), heart failure ( 20% ), ischaemic heart diseases ( 15% ), liver diseases ( 19%) , acute respiratory infections ( 14% ), and diabetes ( 13% ). For middle-aged adults (50–64) in this 13-month period, the relative excess for almost all causes of death examined was higher than that seen for all ages . Deaths involving cardiovascular diseases were 33% higher than expected, while for specific cardiovascular diseases, deaths involving ischaemic heart diseases were 44% higher , cerebrovascular diseases 40% higher and heart failure 39% higher . Deaths involving acute respiratory infections were 43% higher than expected and for diabetes , deaths were 35% higher . Deaths involving liver diseases were 19% higher than expected for those aged 50–64 , the same as for deaths at all ages. Looking at place of death, from 3rd June 2022 to 30th June 2023 there were 22% more deaths in private homes than expected compared with 10% more in hospitals . The greatest numbers of excess deaths in the acute phase of the pandemic were in older adults. The pattern now is one of persisting excess deaths which are most prominent in relative terms in middle-aged and younger adults , with deaths from CVD [cardiovascular] causes and deaths in private homes being most affected.’ ❂ ➲ [C19.Life Note ] : Considering their findings and conclusion, I’m not sure why the authors would choose to use the term ‘post-pandemic’ in this title – when their evidence points to an on-going pandemic, fueled by continuing high rates of infection, that is now simply killing younger age-groups than previously seen.] ❂ 📖 (1 Dec 2023 ~ The Lancet (Regional Health Europe) Excess mortality in England post Covid-19 pandemic: implications for secondary prevention ➤ © 2023 Pearson-Stuttard et al / The Lancet (Regional Health Europe) .
by Outbreak Updates
•
24 November 2023
❦ SARS-CoV-2 infection precipitates a molecular cascade that reactivates latent viral agents. Infection doesn’t just pass through the body’s defenses but rather reprograms them. It reactivates dormant pathogens and perpetuates a cycle of chronic immune activation. Long COVID sufferers are burdened with a significantly higher prevalence of immune responses to certain DNA viruses – namely, Epstein-Barr Virus (EBV)* and Parvovirus B19 – than those in good health. * Epstein-Barr Virus (EBV) is a common human virus that spreads primarily through saliva. It is a member of the herpes virus family and is found all over the world. Most people will get infected with EBV in their lifetime and will not have any symptoms. Elevated levels of antibodies against these viruses in Long COVID patients not only signal potential viral reactivations. It also suggests a reality where SARS-CoV-2 may be inciting a smoldering activation of chronic viral infections. ❂ 📖 (9 Nov 2023 ~ European Heart Journal) Sequential activation of DNA viruses by the RNA virus SARS-CoV-2 in patients with long COVID syndrome ➤ © 2023 Outbreak Updates ➲
by Martin et al / Journal of Neurology
•
7 November 2023
❦ ‘It is now well established that post-COVID syndrome ( PCS ) represents a serious complication in a substantial number of patients following SARS-CoV-2 infection. PCS is diagnosed when COVID-19-related symptoms persist for more than 3 months. It can occur even after an initially mild to moderate course of infection , and comprises a large variety of symptoms . Around 30% of PCS patients show neurological and neuropsychiatric sequelae , such as fatigue , depressive symptoms , and cognitive dysfunction . These are experienced as particularly debilitating, as they have detrimental effects on daily functioning in PCS patients and hamper a successful return to their jobs. Fatigue is a frequent and one of the most debilitating symptoms in post-COVID syndrome (PCS). Recently, we proposed that fatigue is caused by hypoactivity of the brain’s arousal network and reflected by a reduction of cognitive processing speed . Eighty-eight PCS patients with cognitive complaints and 50 matched healthy controls underwent neuropsychological assessment. Seventy-seven patients were subsequently assessed at 6-month follow-up. Patients showed cognitive slowing indicated by longer reaction times compared to control participants in a simple-response tonic alertness task and in all more complex tasks requiring speeded performance . Reduced alertness correlated with higher fatigue . Alertness dysfunction remained unchanged at 6-month follow-up and the same was true for most attention tasks and cognitive domains .’ ❂ 📖 (7 Nov 2023 ~ Journal of Neurology) Persistent cognitive slowing in post-COVID patients: longitudinal study over 6 months ➤ © 2023 Journal of Neurology .
by Rich Haridy / New Atlas
•
31 October 2023
A layperson-level overview from New Atlas on how all variants of SARS-CoV-2 – the virus that causes COVID-19 – are ‘neuroinvasive’ , meaning that all can infect or enter the brain and the nervous system . (From July 2023 Nature Communications study: ‘Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants’.)
by Outbreak Updates
•
11 October 2023
❦ Your brain is a vast city. The roads (myelin) in this city let cars move efficiently. Oligodendrocytes are the construction workers who maintain these roads. As we age, these workers slow down, causing traffic jams and slower thoughts. Enter SARS-CoV-2, the destructive rioter. It doesn’t just disrupt traffic; it damages the roads and chases away the construction crews. Weeks after the riot, the city still struggles to function, with long-lasting road damages and traffic jams. This is the ‘brain fog’ of post-COVID life. ❂ 📖 (24 Sep 2023 ~ Aging and Disease) Role of Microglia, Decreased Neurogenesis and Oligodendrocyte Depletion in Long COVID-Mediated Brain Impairments ➤ © 2023 Outbreak Updates ➲
by Outbreak Updates
•
10 October 2023
❦ Your lungs are balloons made of the finest silk, allowing them to expand and contract effortlessly with each breath. SARS-CoV-2 is as a needle, puncturing and tearing this delicate fabric. In an attempt to heal, the body patches up the punctures, but instead of the original silk, it uses rough patches. These patches – scarring or fibrosis – make parts of the lung rigid, restricting its once flawless expansion. With each subsequent infection, more patches appear, further suffocating the lung’s true function. The virus doesn’t just infect. It sabotages the very essence of our breath. ❂ 📖 (6 Apr 2022 ~ Annals of Medicine and Surgery) Post COVID-19 pulmonary fibrosis; a meta-analysis study ➤ © 2023 Outbreak Updates ➲
by Merck and Co.
•
16 September 2023
❦ ‘The most common causes of acquired lymphocytopenia include: ➲ Protein-energy undernutrition. ➲ HIV infection. ➲ COVID-19 . ➲ Certain other viral infections. Patients with HIV infection routinely have lymphocytopenia, which arises from destruction of CD4+ T cells infected with the HIV virus. Patients with COVID-19 also frequently have lymphocytopenia ( 35% to 83% of patients ) . Lower lymphocyte counts portend a poor prognosis and an increased likelihood of requiring ICU admission and of dying from the disease. The cause of the lymphocytopenia is not completely understood, but COVID-19 can directly infect lymphocytes, and a cytokine-related apoptosis of the cells is likely. ➲ Lymphocytopenia is most often due to AIDS , and recently COVID-19 , or undernutrition, but it also may be inherited or caused by various infections, drugs, or autoimmune disorders. ➲ Patients have recurrent viral , bacterial , fungal , or parasitic infections .’ ❂ 📖 (Accessed 16 Sep 2023 ~ Merck & Co.) Entry for 'Lymphocytopenia' in Merck Manual ➤ © 2023 Merck & Co .
by Sauve et al / eBioMedicine: Lancet Discovery Science
•
12 September 2023
❦ ‘We have recently demonstrated a causal link between loss of gonadotropin-releasing hormone ( GnRH ), the master molecule regulating reproduction , and cognitive deficits during pathological aging , including Down syndrome and Alzheimer’s disease. Olfactory and cognitive alterations , which persist in some COVID-19 patients, and long-term hypotestosteronaemia in SARS-CoV-2-infected men are also reminiscent of the consequences of deficient GnRH, suggesting that GnRH system neuroinvasion could underlie certain post-COVID symptoms and thus lead to accelerated or exacerbated cognitive decline . We explored the hormonal profile of COVID-19 patients and targets of SARS-CoV-2 infection in post-mortem patient brains and human fetal tissue. We found that persistent hypotestosteronaemia in some men could indeed be of hypothalamic origin , favouring post-COVID cognitive or neurological symptoms , and that changes in testosterone levels and body weight over time were inversely correlated. Infection of olfactory sensory neurons and multifunctional hypothalamic glia called tanycytes highlighted at least two viable neuroinvasion routes . Furthermore, GnRH neurons themselves were dying in all patient brains studied , dramatically reducing GnRH expression. Human fetal olfactory and vomeronasal epithelia , from which GnRH neurons arise, and fetal GnRH neurons also appeared susceptible to infection . Putative GnRH neuron and tanycyte dysfunction following SARS-CoV-2 neuroinvasion could be responsible for serious reproductive , metabolic , and mental health consequences in long-COVID and lead to an increased risk of neurodevelopmental and neurodegenerative pathologies over time in all age groups .’ ❂ 📖 (12 Sep 2023 ~ eBioMedicine: Lancet Discovery Science) Long-COVID cognitive impairments and reproductive hormone deficits in men may stem from GnRH neuronal death ➤ © 2023 eBioMedicine: Lancet Discovery Science .
by Antiviral Marketing
•
11 September 2023
❦ — “I don’t know anyone with Long Covid.” — “Everyone I know is tired.” ❂ © 2023 Antiviral Marketing . ➲
by Di Chiara et al / Acta Paediatrica
•
9 September 2023
❦ Children have largely been unaffected by severe COVID-19 compared to adults, but data suggest that they may have experienced new conditions after developing the disease. We compared 1656 exposed and 1656 unexposed children from 1 February 2020 to 30 November 2021. We found significantly higher risks for some new conditions in exposed children, including mental health issues and neurological problems . The overall excess risk for new-onset conditions after COVID-19 was 78% higher in the exposed than unexposed children. ❂ 📖 (9 Sep 2023 ~ Acta Paediatrica) Comparative study showed that children faced a 78% higher risk of new-onset conditions after they had COVID-19 ➤ © 2023 Di Chiara et al / Acta Paediatrica.
by Parotto et al / The Lancet
•
17 July 2023
❦ ‘Individuals with SARS-CoV-2 infection can develop symptoms that persist well beyond the acute phase of COVID-19 or emerge after the acute phase, lasting for weeks or months after the initial acute illness. The post-acute sequelae of COVID-19 (PASC) , which include physical, cognitive, and mental health impairments, are known collectively as long COVID or post-COVID-19 condition (PCC) . The proportion of patients affected by post-COVID-19 condition might be in the range of 10–30% of those infected with SARS-CoV-2, although understanding of this condition is still evolving. Socio-economic factors are fundamental determinants of health after COVID-19. Individuals from low-income and middle-income countries, those from marginalised communities, and those who are socially disadvantaged are probably disproportionately affected. The post-COVID-19 condition is systemic, affecting various organ systems. PCC results in: an increased use of healthcare resources ; a decreased quality of life ; an increased susceptibility to subsequent viral or bacterial infection ; and leads to heightened vulnerability to perioperative morbidity and mortality for individuals who require a surgical procedure for any (unrelated) indication. With a large and growing global population of survivors of COVID-19, the impact on individuals, healthcare systems, communities, and society is likely to be substantial. At present, there are no specific treatments for post-COVID-19-condition.’ ❂ 📖 (17 July 2023 ~ The Lancet) Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations ➤ © 2023 Parotto et al / The Lancet.
by Altmann et al / Nature
•
11 July 2023
❦ ‘Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new healthcare challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with Long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein-Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. The oncoming burden of Long COVID faced by patients, healthcare providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it.’ ❂ 📖 (11 July 2023 ~ Nature Reviews: Immunology) The immunology of long COVID ➤ © 2023 Altmann et al / Nature.
by Dr. Kelly Fearnley, NHS (England)
•
4 July 2023
‘Healthcare workers must be provided with respiratory protection and the air quality in hospitals be monitored and improved through the installation of ventilation systems and air filter units.’ ✾
by NHS Palliative Care Medicine Consultant
•
25 June 2023
❦ “Feeling validated that life is ‘back to normal’ as you see all of those unmasked people around you in restaurants, shops and cinemas? I’ll let you in on a little secret. Those who recognise the risk and who would be masked up aren’t even there. They are busy elsewhere staying healthy. More than 400 million now have Long Covid; a disease from Covid that can impact any organ system, and is proven to cause damage to the brain, heart, lung, kidney, gut, immune and multiple other systems. That’s one in 20 globally. How come you don’t know anyone with it? It’s one of three likely reasons… 1. They have been sick so long that they do what most chronically ill people do when they are asked, “How are you?” They say, “I’m fine”. 2. They don’t recognise the relation of their recent heart attack/memory impairment/new diabetes to their Covid illness in the last year. 3. It’s because they aren’t at that restaurant, movie, theatre, work night out as they don’t fancy worsening their already awful situation with a further infection. Out of sight, out of mind. Even those who know someone with Long Covid will minimise it, as it doesn’t fit with the general narrative that Covid is over. It’s too much cognitive dissonance for most people to handle. Easier to believe that everything’s OK, and it must “just be them being anxious”. It’s not over. I’ll let you in on another special secret; it’s not anxiety. It’s a calm determination to maintain health, in the full knowledge of what Covid can do.” © 2023 NHS Palliative Care Medicine Consultant .
by NHS Medical Consultant
•
25 June 2023
❦ I have seen a disproportionate number of young patients with advanced cancer over the last two years. They used to stand out: now it’s every week. The evidence points to direct Covid-driven mechanisms for rises in cancer risk. Will you hear about it in the news? Of course not. Covid’s over. It’s just anxiety now if you’re thinking about it. Except it’s not. It’ll take years for people to accept this. It’ll be too late. A number of my oncology colleagues have been commenting on how they’ve never seen such aggressively-progressive cancers in all their careers since Covid arrived. I’ve been seeing it as all these patients come to me. It isn’t normal. Alarm bells should be ringing loudly. The evidence: 📖 (22 Mar 2023 ~ Global Journal of Life Sciences and Biological Research) Cancer Related-Genes Enriched in Peripheral Blood Mononuclear Cells (PBMCs) of COVID-19 Patients: A Bioinformatics Study ➤ ‘SARS-CoV-2 can be considered a potential risk factor for increasing the probability of developing cancer.’ Study 1: 📖 (7 Jun 2022 ~ Frontiers in Oncology) SARS-CoV-2 M Protein Facilitates Malignant Transformation of Breast Cancer Cells ➤ ‘Coronavirus disease 2019 (COVID-19) has spread faster due to the emergence of SARS-CoV-2 variants, which carry an increased risk of infecting patients with comorbidities, such as breast cancer.’ Study 2: 📖 (9 Aug 2022 ~ Journal of Infection ) Is SARS-CoV-2 an oncogenic virus? ➤ ‘Gene expression of p53 [tumour suppressor] is downregulated in blood of COVID-19 patients. Downregulation persists at least 24 weeks after infection in long COVID-19 patients. Long-term reduction of p53 could have impact on carcinogenesis.’ 📖 (9 Aug 2022 ~ Journal of Infection) Letter to the editor: Is SARS-CoV-2 an oncogenic virus? ➤ Study 3: 📖 (22 Mar 2023 ~ Global Journal of Life Sciences and Biological Research) Cancer related-genes enriched in peripheral blood mononuclear cells (PBMCs) of COVID-19 patients. A bioinformatics study ➤ ‘Numerous cancer-related genes up-regulated in SARS-CoV-2-infected patients, particularly those genes participating in the cell-cycle regulation or engaged in cellular senescence processes.’ Study 4: 📖 (2 Jun 2023 ~ Biochimie) Possible cancer-causing capacity of COVID-19: Is SARS-CoV-2 an oncogenic agent? ➤ ‘One of the most worrying long-term effects of infection is the potential to induce malignant neoplasms, which will be a major health concern over the coming decades. SARS-CoV-2 infection affects many mechanisms that play a crucial role in cancer onset and progression including cell-cycle regulation, the RAAS system and inflammation / proliferation signaling pathways.’ ❂ Related reading : 📖 (9 Aug 2021 ~ Nature: Scientific Reports) More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis ➤ 📖 (21 Jun 2021 ~ Nature: Scientific Reports) The risk of pancreatic adenocarcinoma following SARS-CoV family infection ➤ 📖 (4 Mar 2021 ~ Nature: Scientific Reports) COVID-19 engages clinical markers for the management of cancer and cancer-relevant regulators of cell proliferation, death, migration, and immune response ➤ 📖 (28 Jan 2021 ~ Nature: Scientific Reports) Meta-analysis of host transcriptional responses to SARS-CoV-2 infection reveals their manifestation in human tumors ➤ 📖 (25 Jan 2010 ~ Nature: Oncogene) Viral epigenome in human tumorigenesis ➤ 📖 (Dec 2006 ~ Yale Journal of Biology and Medicine) Viruses and human cancer ➤ ❂ © 2023 NHS Medical Consultant .
by Martinez-Marmol & Hilliard / Queensland Brain Institute
•
8 June 2023
❦ Researchers at The University of Queensland have discovered viruses such as SARS-CoV-2 can cause brain cells to fuse, initiating malfunctions that lead to chronic neurological symptoms. SARS-CoV-2, the virus that causes COVID-19, has been detected in the brains of people with 'Long COVID' months after their initial infection. "We discovered COVID-19 causes neurons to undergo a cell fusion process, which has not been seen before," Professor Hilliard said. "After neuronal infection with SARS-CoV-2, the spike S protein becomes present in neurons, and once neurons fuse, they don't die." "They either start firing synchronously, or they stop functioning altogether." As an analogy, Professor Hilliard likened the role of neurons to that of wires connecting switches to the lights in a kitchen and a bathroom. "Once fusion takes place, each switch either turns on both the kitchen and bathroom lights at the same time, or neither of them," he said. "It's bad news for the two independent circuits." The discovery offers a potential explanation for persistent neurological effects after a viral infection. "In the current understanding of what happens when a virus enters the brain, there are two outcomes – either cell death or inflammation," Dr Martinez-Marmol said. "But we've shown a third possible outcome, which is neuronal fusion." Dr Martinez-Marmol said numerous viruses cause cell fusion in other tissues, but also infect the nervous system and could be causing the same problem there. "These viruses include HIV, rabies, Japanese encephalitis, measles, herpes simplex virus and Zika virus," he said. “Our research reveals a new mechanism for the neurological events that happen during a viral infection. “This is potentially a major cause of neurological diseases and clinical symptoms that is still unexplored.” ❂ 📖 (7 June 2023 ~ Science Advances) SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity ➤ 📖 (8 June 2023 ~ Queensland Brain Institute) COVID-19 can cause brain cells to 'fuse' ➤ © 2023 Martinez-Marmol & Hilliard / Queensland Brain Institute / University of Queensland.
by NHS Palliative Medicine Consultant
•
19 May 2023
❦ “What if Covid has been causing mass cognitive impairment and we are all living in an increasingly stupid society? Mad things could happen with that: imagine if hospitals got rid of masks or people started to believe Covid was just a cold? I know that’s far-fetched, but imagine!” ❂ © 2023 NHS Palliative Medicine Consultant .
by The John Snow Project
•
5 May 2023
❦ Prior to 2020, there were four endemic human coronaviruses – OC43, NL-63, 229E, and HKU1 – which were known to cause 10 to 15 percent of common colds – or the ‘Common Cold Coronaviruses’ (CCCs). From at least the 1970s, we’ve known that infection with these coronaviruses does not lead to lasting protection from reinfection – this is textbook knowledge. CCCs are not just colds – they can cause severe pneumonias, and exhibit a risk profile very similar to SARS-CoV-2 with age. If reinfection really did strengthen immunity against CCCs, then older people would be the least affected – because they would have been regularly infected with diverse variants of these viruses in their past. But that is not the case – and SARS-CoV-2 is not a CCC. SARS-CoV-2 has a wide array of accessory proteins that silence and disrupt our normal immune responses. As we get older, our immune systems start to lose their effectiveness – and we become more susceptible to disease. This process is called immunosenescence . Repeated exposure to a virus like SARS-CoV-2 is fast-tracking more people into immunosenescence at ever-earlier ages, with potentially serious repercussions for their health and longevity. SARS-CoV-2 is a particularly nasty virus that can also trigger the hyperactivation of our own immune systems to cause severe disease. Infection by SARS-CoV-2 has been shown to lead to an increase in autoantibodies and autoimmune disease. Approximately 25 percent of people who develop an autoimmune disease will experience multiple autoimmune syndrome, and will risk a cascade of autoimmune conditions. SARS-CoV-2, like its 2002 predecessor SARS-CoV-1, is both a respiratory and a systemic virus, with an extremely broad cell-type and tissue-tropism covering nearly the whole body. Its ability to infect and do damage to lungs, hearts, kidneys, cardiovascular systems and brains is particularly well-documented. If each subsequent infection results in additional internal organ and immune-system damage, then at some point the damage accumulated – together with the accelerated immune-system aging and normal aging processes – can reasonably be expected to outweigh the protective benefits of immunity developed from previous infections. SARS-CoV-2 reinfects more frequently than influenza or the common cold, infects a wider range of organs, does more damage and seems capable of persisting in a range of organs. So if SARS-CoV-2 behaves like a textbook virus – but does more damage more quickly and more regularly – at what point does the body reach its tipping point? ❂ There are two versions of this article: a 7-minute read in simplified language ; and the full editorial version complete with references, which is an 18-minute-read and aimed towards the medical and scientific communities . ❦ 7-minute primer ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❦ Full 18-minute editorial ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❂ 📖 (5 May 2023 ~ The John Snow Project) SARS-CoV-2 and "Textbook" Immunity ➤ © 2023 The John Snow Project.
by Costanzo et al / International Journal of Molecular Sciences
•
25 April 2023
❦ ‘Some viruses are known to be associated with the onset of specific cancers. These micro-organisms – oncogenic viruses or oncoviruses – can convert normal cells into cancer cells. Seven oncogenic viruses are known to promote tumorigenesis [tumour creation] in humans: Human papillomavirus (HPV) Hepatitis B and C viruses (HBV, HCV) Epstein-Barr virus (EBV) Human T-cell leukemia virus 1 (HTLV-1) Kaposi sarcoma-associated herpesvirus (KSHV) Merkel cell polyomavirus (MCPyV) Recent research indicates that SARS-CoV-2 infection and COVID-19 progression may predispose recovered patients to cancer onset and accelerate cancer development . This hypothesis is based on the growing evidence regarding the ability of SARS-CoV-2 to modulate oncogenic pathways, promoting chronic low-grade inflammation and causing tissue damage.’ ❂ 📖 (25 Apr 2023 ~ International Journal of Molecular Sciences) Deciphering the Relationship between SARS-CoV-2 and Cancer ➤ © 2023 Costanzo et al / International Journal of Molecular Sciences.
by Negm et al / BMC Infectious Diseases
•
23 April 2023
❦ Critically ill COVID-19 patients are highly susceptible to opportunistic fungal infection due to many factors, including virus-induced immune dysregulation , host-related comorbidities, overuse and misuse of antibiotics or corticosteroids, immune modulator drugs, and the emergencies caused by the pandemic. Fungal coinfection is a common complication of critically ill COVID-19 patients admitted to the ICU. Candidiasis , aspergillosis , and mucormycosis are the most common COVID-19-associated fungal infections and have a great impact on mortality rates . ❂ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ © 2023 Negm et al / BMC Infectious Diseases.
by Herrera et al / Nature: Scientific Reports
•
19 April 2023
❦ The results presented here reveal that at least 85% [of the 214 patients with post COVID-19 syndrome] exhibit deficits in one neuropsychological test . Also, the youngest patients were those who showed the most marked and heterogeneous cognitive impairment , while the oldest patients maintained their cognitive functions preserved to a greater extent with only a mild impairment in attention and speed processing. ❂ 📖 (19 Apr 2023 ~ Nature: Scientific Reports) Cognitive impairment in young adults with post COVID-19 syndrome ➤ © 2023 Herrera et al / Nature.
by Sayyadi et al / Annals of Hematology
•
19 April 2023
❦ ‘COVID-19 patients have a hypercoagulability state, and thrombosis is a life-threatening complication of them.’ ✻ Hypercoagulability , also known as thrombophilia , is a condition in which there is an abnormally increased tendency towards blood clotting . ‘From the early days of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) outbreak to the present, clinical and basic studies have indicated that coronavirus disease 2019 (COVID-19) may be associated with coagulopathy ( CAC ), which is involved in its related morbidity and mortality. Deep vein thrombosis ( DVT ) and pulmonary embolism ( PE ) are common in COVID-19 patients and are remarkably high in the intensive care unit (ICU)–admitted patients. CAC can lead to the formation of circulating microthrombi and macrothrombi which can involve multiple sites, including the lungs , brain , heart , and visceral organs like kidneys and spleen . There is a close relationship between the immune system and coagulation. The components of the hemostatic system play a role in the body’s immunity, and the activation of the immune system strongly influences the hemostatic system. Abnormal activation of the immune system may promote the growth of pathologies associated with thrombosis. COVID-19 is accompanied by an immune-cell hyperactivation and excessive production of proinflammatory cytokines , known as “ cytokine storm ”. CAC is theorized to result from dysregulated interactions between the immune and coagulation systems .’ ❂ 📖 (19 Apr 2023 ~ Annals of Hematology) Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement ➤ © 2023 Annals of Hematology .
by Chen et al / Journal of Medical Virology
•
18 April 2023
❦ 'The risk of herpes zoster (HZ) [ shingles ] remained significantly higher [ +60% ] in patients with COVID-19, compared with those without COVID-19. The higher risk of HZ in the COVID-19 cohort compared with that in the non-COVID-19 cohort remained consistent across subgroup analyses regardless of vaccine status, age, or sex. The risk of HZ within a 12-month follow-up period was significantly higher in patients who had recovered from COVID-19 compared with that in the control group.' ❂ 📖 (18 Apr 2023 ~ Journal of Medical Virology) Long-term risk of herpes zoster following COVID-19: A retrospective cohort study of 2 442 686 patients ➤ © 2023 Journal of Medical Virology.
by Wang et al / International Journal of Molecular Sciences
•
18 April 2023
❦ ‘Pulmonary arterial hypertension (PAH) is a pulmonary vascular disease characterized by the progressive elevation of pulmonary arterial pressures.’ Pulmonary Arterial Hypertension ( PAH ) is a progressive lung disease that affects the heart and lungs . It is caused when the tiny arteries in the lungs become thickened and narrowed , causing abnormally high blood pressure in the pulmonary artery . Symptoms include shortness of breath during exercise, fainting spells , dizziness , swelling of the ankles or legs , chest pain , and a racing pulse . ‘It is becoming increasingly apparent that inflammation contributes to the pathogenesis and progression of PAH. Several viruses are known to cause pulmonary arterial hypertension (PAH) , such as SARS-CoV-2 , Human Endogenous Retrovirus K (HERV-K), and Human Immunodeficiency Virus ( HIV ), in part due to acute and chronic inflammation .’ ❂ 📖 (18 Apr 2023 ~ International Journal of Molecular Sciences) Human Endogenous Retrovirus, SARS-CoV-2, and HIV Promote PAH via Inflammation and Growth Stimulation ➤ © 2023 International Journal of Molecular Sciences .
by Sharma & Jagadeesh / Nature Reviews: Rheumatology
•
12 April 2023
❦ The full picture of post-COVID-19 autoimmune diseases and their prevalence is lacking despite numerous case reports and small series. Two studies that use large cohorts now highlight that SARS-CoV-2 infection is linked to a substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases . The reports by Chang et al and Tesch et al provide a comprehensive overview of diverse new-onset autoimmune conditions after COVID-19. In addition, an earlier preprint of a retrospective matched cohort analysis using data from the Clinical Practice Research Datalink Aurum database of 458,147 SARS-CoV-2-infected and 1,818,929 uninfected adults across England between 31 January 2020 and 30 June 2021 reported that the incidence of type 1 diabetes mellitus , inflammatory bowel disease and psoriasis are significantly associated with SARS-CoV-2 infection. Some of the earliest evidence that SARS-CoV-2 infection leads to dysregulated immune responses came from paediatric patients who presented with multisystem inflammatory syndrome in children (MIS-C) , which, as the name indicates, involves diffuse organ system involvement and a clinical spectrum that overlaps with other hyperinflammatory syndromes , such as Kawasaki disease , toxic-shock syndrome , and macrophage activation syndrome . Since the start of the pandemic, many researchers have also reported isolated cases of adults with various post-COVID-19 autoimmune conditions. ❂ 📖 (12 Apr 2023 ~ Nature Reviews: Rheumatology) High risk of autoimmune diseases after COVID-19 ➤ © 2023 Sharma & Jagadeesh / Nature.
by Linseman Laboratory / University of Denver
•
4 April 2023
❦ The Linseman Laboratory is studying the long-term brain health effects of COVID-19 in individuals with and without traumatic brain injury (TBI). Preliminary data suggest that those with a history of both COVID-19 and TBI experience more severe Long COVID symptoms, a higher symptom burden , and more frequent symptoms . Those who reported having COVID-19 and TBI reported worse depressive symptoms , worse functional outcomes , and increased fatigue . ❂ 📖 (4 Apr 2023 ~ SciTechDaily) Researchers Discover Connection Between Traumatic Brain Injury and Long COVID ➤ © 2023 Linesman Laboratory / University of Denver / SciTechDaily.