on immunity
“People do become very worried if you compare COVID-19 to HIV, but actually HIV has good treatment and life expectancy now.”
Dr. Noor Bari, Emergency Medicine (2023)
❦ on three scenarios
“COVID-19 is fighting back by generally depressing the whole adaptive immune system.
We are showing narrow resilience to COVID reinfections due to adapting – but we are becoming more vulnerable in general to infections of all kinds.
➲ Worst case scenario
A single infection causes on-going and progressive immunodeficiency.
➲ Best case scenario
A single infection causes temporary immunosuppression, and we suppress COVID transmission enough to allow recovery.
➲ Most likely scenario, medium-term
Immunosuppression that becomes continuous and possibly progressive due to reinfections.
Reduced immune function after a viral infection is not unusual.
Many viruses do this.
The concerning issue is the length and breadth of the immune system dysfunction, coupled with emerging evidence of other pathogens taking advantage.”
Dr. Noor Bari, Emergency Medicine (2023)
❦ Immunosuppression ~ Suppression of the immune system and its ability to fight infection.
❦ Immunodeficiency ~ A state in which the immune system’s ability to fight infectious diseases and cancer is compromised, or entirely absent.
❦ on repeated exposure
‘Repeated exposure to a virus such as SARS-CoV-2 will fast-track more people into immunosenescence at ever-earlier ages, with potentially serious repercussions for their health and longevity.’
The John Snow Project (2023)
❦ Immunosenescence ~ The gradual deterioration of the immune system, normally brought on by natural age advancement.
Immunosenescence is closely related to the development of infections, autoimmune diseases, and malignant tumors.
❦ on lymphocytopenia
The most common causes of acquired lymphocytopenia include:
➲ Protein-energy undernutrition.
➲ HIV infection.
➲ COVID-19.
➲ Certain other viral infections.
Patients with HIV infection routinely have lymphocytopenia, which arises from destruction of CD4+ T cells infected with the HIV virus.
➲ Patients with
COVID-19
also frequently have
lymphocytopenia
(35%
to
83%
of patients).
➲ Patients have recurrent viral, bacterial, fungal, or parasitic infections.
Merck Manual ➲ (2023)
❦ on the hygiene hypothesis, and pathogenic viruses
‘The hygiene hypothesis is the idea that the immune system needs to be “trained” during childhood to properly develop immune tolerance to microbes, but it specifically refers to bacteria, protozoans and helminths, most of which are normally beneficial, neutral or not significantly harmful to humans.
It does not advocate repeated exposure to viruses, especially highly pathogenic ones.’
The John Snow Project (2023)
❦ immunity ~ further reading
C-19 Archives:
immunity
























❦ on immunity: scientific papers & media articles
✒ 2023
📖 (Accessed 20 Sep 2023 ~ University of Oxford) Autoimmune disorders found to affect around one in ten people ➤
❂
📖 (13 Sep 2023 ~ 1 News/NZ) Covid may have permanently damaged people's immunity ➤
❂
📖 (18 Aug 2023 ~ Cell) Epigenetic memory of coronavirus infection in innate immune cells and their progenitors ➤
❂
📖 (16 Aug 2023 ~ The Lancet / eClinicalMedicine) Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study ➤
❂
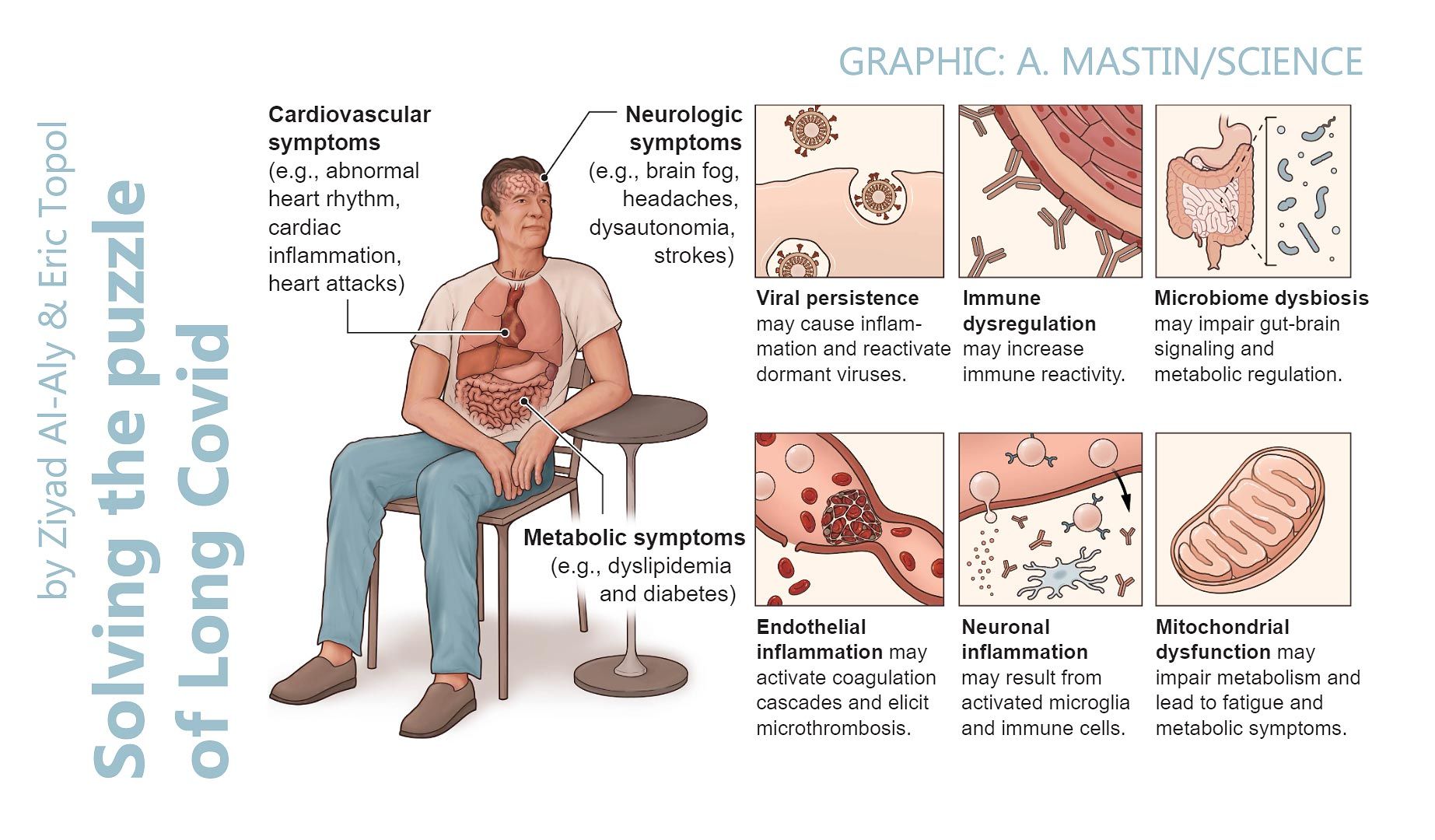
📖 (9 Aug 2023 ~ Science: Translational Medicine) Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts ➤
❂
📖 (4 Aug 2023 ~ Pre-print) Long COVID manifests with T cell dysregulation, inflammation, and an uncoordinated adaptive immune response to SARS-CoV-2 ➤
❂
📖 (19 Jun 2023 ~ Clinical Rheumatology) Incident autoimmune diseases in association with SARS-CoV-2 infection: a matched cohort study ➤
❂
📖 (3 Jun 2023 ~ The Lancet) Incidence, prevalence, and co-occurrence of autoimmune disorders over time and by age, sex, and socioeconomic status: a population-based cohort study of 22 million individuals in the UK ➤
❂
📖 (3 May 2023 ~ Infectious Diseases) Evaluation of Waning of SARS-CoV-2 Vaccine-Induced Immunity – A Systematic Review and Meta-analysis ➤
❂
📖 (25 Apr 2023 ~ International Journal of Molecular Sciences) Deciphering the Relationship between SARS-CoV-2 and Cancer ➤
➲ 'Some viruses are known to be associated with the onset of specific cancers.
These micro-organisms, oncogenic viruses or oncoviruses, can convert normal cells into cancer cells by modulating the central metabolic pathways or hampering genomic integrity mechanisms, consequently inhibiting the apoptotic machinery and/or enhancing cell proliferation.
Seven oncogenic viruses are known to promote tumorigenesis [the formation of a cancer] in humans: human papillomavirus (HPV) [associated with genital warts], hepatitis B and C viruses (HBV, HCV), Epstein-Barr virus (EBV) [human herpesvirus 4], human T-cell leukemia virus 1 (HTLV-1), Kaposi sarcoma-associated herpesvirus (KSHV), and Merkel cell polyomavirus (MCPyV).
Recent research indicates that SARS-CoV-2 infection and COVID-19 progression may predispose recovered patients to cancer onset and accelerate cancer development.'
❂
📖 (18 Apr 2023 ~ Journal of Medical Virology) Long-term risk of herpes zoster following COVID-19: A retrospective cohort study of 2 442 686 patients ➤
➲ 'The risk of herpes zoster (HZ) (Shingles) remained significantly [+60%] higher in patients with COVID-19 compared with those without COVID-19.
The higher risk of HZ in the COVID-19 cohort compared with that in the non-COVID-19 cohort remained consistent across subgroup analyses regardless of vaccine status, age, or sex.
The risk of HZ within a 12-month follow-up period was significantly higher in patients who had recovered from COVID-19 compared with that in the control group.'
❂
📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤
➲ 'Critically ill COVID-19 patients are highly susceptible to opportunistic fungal infection due to many factors, including virus-induced immune dysregulation, host-related comorbidities, overuse and misuse of antibiotics or corticosteroids, immune modulator drugs, and the emergencies caused by the pandemic.
Fungal coinfection is a common complication of critically ill COVID-19 patients admitted to the ICU. Candidiasis, aspergillosis, and mucormycosis are the most common COVID-19-associated fungal infections and have a great impact on mortality rates.'
❂
📖 (14 Apr 2023 ~ Viruses) SARS-CoV-2 Reinfection and Severity of the Disease: A Systematic Review and Meta-Analysis ➤
➲ 'Reinfection with SARS-CoV-2 does occur, suggesting that natural immunity is not long-lasting in COVID-19 patients. Female patients seem more likely to experience reinfection than male patients.
Thus far, no clear evidence for a difference in severity between the first infection and reinfection has been observed.'
❂
📖 (12 Apr 2023 ~ Nature Reviews: Rheumatology) High risk of autoimmune diseases after COVID-19 ➤
➲ 'Two studies that use large cohorts now highlight that SARS-CoV-2 infection is linked to a substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases.
The reports by Chang et al and Tesch et al provide a comprehensive overview of diverse new-onset autoimmune conditions after COVID-19.
In addition, an earlier preprint of a retrospective matched cohort analysis using data from the Clinical Practice Research Datalink Aurum database of 458,147 SARS-CoV-2-infected and 1,818,929 uninfected adults across England between 31 January 2020 and 30 June 2021 reported that the incidence of type 1 diabetes mellitus, inflammatory bowel disease and psoriasis are significantly associated with SARS-CoV-2 infection.'
❂
📖 (21 Mar 2023 ~ Infection Control Today) COVID-19: Study Suggests Long-term Damage to Immune System ➤
❂
📖 (March 2023 ~ Asia Pacific Allergy) Immunological dysfunction and mast cell activation syndrome in long COVID ➤
❂
📖 (16 Feb 2023 ~ BMC Biology) High SARS-CoV-2 tropism and activation of immune cells in the testes of non-vaccinated deceased COVID-19 patients ➤
❂
📖 (7 Feb 2023 ~ Journal of Allergy and Clinical Immunology) SARS-CoV-2 infection of thymus induces loss of function that correlates with disease severity ➤
➲ 'Lymphopenia, particularly when restricted to the T-cell compartment, has been described as one of the major clinical hallmarks in patients with coronavirus disease 2019 (COVID-19) and proposed as an indicator of disease severity.
Although several mechanisms fostering COVID-19-related lymphopenia have been described, including cell apoptosis and tissue homing, the underlying causes of the decline in T-cell count and function are still not completely understood.
Patients with COVID-19 had reduced thymic function that was inversely associated with the severity of the disease.
Our data demonstrate that the human thymus is a target of SARS-CoV-2 and thymic function is altered following infection.'
Note: Lymphopenia (also called lymphocytopenia) is a disorder in which your blood doesn't have enough white blood cells called lymphocytes. Lymphocytes play a protective role in your immune system.
❂
📖 (18 Jan 2023 ~ Nature) How your first brush with COVID warps your immunity ➤
❂
📖 (13 Jan 2023 ~ Preprint) Structure-based discovery of inhibitors of the SARS-CoV-2 Nsp14 N7-methyltransferase ➤
❂
📖 (12 Jan 2023 ~ News-Medical.Net) New insights into deadly fungal invasion in people with compromised immune systems ➤
➲ 'Fungi such as Aspergillus are so common in our surroundings that we breathe in hundreds to thousands of spores every day.
In healthy people, fungi typically pose no threat, but they can cause deadly infections in those with compromised immune systems.
However, it is increasingly recognized that viral infections such as influenza or SARS-CoV-2 can increase the risk of invasive Aspergillus infections even in healthy people.'
❂
📖 (11 Jan 2023 ~ Nature Reviews: Immunology) Innate immune evasion strategies of SARS-CoV-2 ➤
❂
📖 (January 2023 ~ Clinical Immunology) Tracking the clonal dynamics of SARS-CoV-2-specific T cells in children and adults with mild/asymptomatic COVID-19 ➤
❂
✒ 2022
📖 (26 Dec 2022 ~ Nature) Transcriptional reprogramming from innate immune functions to a pro-thrombotic signature by monocytes in COVID-19 ➤
❂
📖 (6 Dec 2022 ~ Best Practice & Research Clinical Haematology) COVID-19 disease and immune dysregulation ➤
➲ 'While COVID-19 was originally characterized as hyperinflammatory in its pathophysiology, emerging evidence demonstrates the possibility of a strongly immunosuppressive phenotype in more critical disease states.
While immune activation from neutrophils and complement may contribute to inflammatory damage in the lungs, decreased antiviral responses, dysregulated macrophages and dendritic cells, and severe lymphopenia contribute to a suppressed state in which viral replication and secondary infections are prone.'
❂
Note: ❊ = Scientific paper illustrating clear immune dysregulation.
❊ 📖 (2 Dec 2022 ~ Frontiers in Immunology) Single-cell multiomics revealed the dynamics of antigen presentation, immune response and T cell activation in the COVID-19 positive and recovered individuals ➤
❂
❊ 📖 Preprint: (20 Nov 2022 ~ medRxiv) Direct Cryo-ET observation of platelet deformation induced by SARS-CoV-2 Spike protein ➤
❂
❊ 📖 Preprint: (20 Nov 2022 ~ medRxiv) Elevated circulating monocytes and monocyte activation in pulmonary post-acute sequelae of SARS-CoV-2 infection ➤
❂
📖 (22 Oct 2022 ~ Cleveland.com) In Cleveland and beyond researchers begin to unravel the mystery of long COVID-19 ➤
❂
📖 (7 Oct 2022 ~ Counter Disinformation Project) "Immunity Debt"? Established 2021 ➤
❂
📖 (22 Sep 2022 ~ European Respiratory Journal) Circulating anti-nuclear autoantibodies in COVID-19 survivors predict long COVID symptoms ➤
❂
📖 (12 Sep 2022 ~ Nature: Communications) Previous immunity shapes immune responses to SARS-CoV-2 booster vaccination and Omicron breakthrough infection risk ➤
❂
📖 (17 Aug 2022 ~ The Conversation) When COVID-19 or flu viruses kill, they often have an accomplice – bacterial infections ➤
➲ 'The 1918 influenza pandemic resulted in the loss of over 3% of the world's population – at least 50 million people.
But it wasn't the flu virus that caused the majority of these deaths.
An analysis of lung samples collected during that flu pandemic indicated that most of the deaths were likely due to bacterial pneumonia, which ran rampant in the absence of antibiotics.
Even in more recent history, like the 1957 H2N2 and 2009 H1N1 flu pandemics, nearly 18% of patients with viral pneumonia had additional bacterial infections that increased their risk of death.
And the COVID-19 pandemic is no different.'
❂
📖 (PDF) (4 Aug 2022 ~ European Respiratory Journal) Circulating anti-nuclear autoantibodies in COVID-19 survivors predict long COVID symptoms ➤
❂
📖 (14 May 2022 ~ Allergy) T-cell recovery and evidence of persistent immune activation 12 months after severe COVID-19 ➤
❂
📖 (1 May 2022 ~ Gastroenterology) Postacute COVID-19 is Characterized by Gut Viral Antigen Persistence in Inflammatory Bowel Diseases ➤
❂
📖 (22 Apr 2022 ~ Clinical Infectious Diseases) Reduced Cell Surface Levels of C-C Chemokine Receptor 5 and Immunosuppression in Long Coronavirus Disease 2019 Syndrome ➤
❂
📖 (8 Apr 2022 ~ Pre-print) SARS-CoV-2 and its variants, but not Omicron, induces thymic atrophy and impaired T cell development ➤
❂
📖 (23 Mar 2022 ~ Pathogens) Superantigens and SARS-CoV-2 ➤
❂
❊ 📖 (11 Mar 2022 ~ Nature Signal Transduction and Targeted Therapy) ACE2-independent infection of T lymphocytes by SARS-CoV-2 ➤
❂
📖 (10 Mar 2022 ~ Science) The immunology and immunopathology of COVID-19 ➤
❂
📖 (3 Mar 2022 ~ Frontiers) Understanding the Effects of Age and T-Cell Differentiation on COVID-19 Severity: Implicating a Fas/FasL-mediated Feed-Forward Controller of T-Cell Differentiation ➤
❂
❊ 📖 (21 Feb 2022 ~ Frontiers in Immunology) Depletion and Dysfunction of Dendritic Cells: Understanding SARS-CoV-2 Infection ➤
❂
❊ 📖 (22 Jan 2022 ~ Nature Immunology) Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection ➤
❂
❊ 📖 (14 Jan 2022 ~ BMC Medicine) Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection ➤
❂
📖 (13 Jan 2022 ~ Nature) Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection ➤
❂
✒ 2021
📖 (16 Nov 2021 ~ The Journal of Clinical Investigation) PD-1 blockade counteracts post-COVID-19 immune abnormalities and stimulates the anti-SARS-CoV-2 immune response ➤
❂
📖 (1 Oct 2021 ~ Pathogens) Uncertainty around the Long-Term Implications of COVID-19 ➤
❂
❊ 📖 (22 Sep 2021 ~ Nature / Signal Transduction and Targeted Therapy) SARS-CoV-2 infection causes immunodeficiency in recovered patients by downregulating CD19 expression in B cells via enhancing B-cell metabolism ➤
❂
❊ 📖 (21 July 2021 ~ Nature / Cellular & Molecular Immunology) Dendritic cell deficiencies persist seven months after SARS-CoV-2 infection ➤
❂
📖 (25 May 2021 ~ The Journal of Clinical Investigation) Multisystem inflammatory syndrome in children is driven by zonulin-dependent loss of gut mucosal barrier ➤
❂
📖 (7 May 2021 ~ Frontiers in Immunology) Longitudinal Analysis of COVID-19 Patients Shows Age-Associated T Cell Changes Independent of Ongoing Ill-Health ➤
❂
📖 (20 Apr 2021 ~ Autoimmunity Reviews) Granulomatous manifestations associated with COVID19 infection: Is there a link between these two diseases? ➤
➲ 'Covid infections are putting people at higher risk of diabetes, strokes, heart disease and other long-term illnesses – but experts warn it may be decades before the full impact is known.'
❂
📖 (21 Mar 2021 ~ Journal of Cosmetic Dermatology) Oral candidiasis of COVID‐19 patients: Case report and review of evidence ➤
❂
📖 (11 Mar 2021 ~ The Journal of Clinical Investigation) HLA class I-associated expansion of TRBV11-2 T cells in multisystem inflammatory syndrome in children ➤
❂
📖 (4 Mar 2021 ~ KFF Health News) Coronavirus Deranges the Immune System in Complex and Deadly Ways ➤
➲ 'While all viruses find ways to evade the body's defenses, a growing field of research suggests that the coronavirus unhinges the immune system more profoundly than previously realized.
Some covid survivors have developed serious autoimmune diseases, which occur when an overactive immune system attacks the patient, rather than the virus.
Doctors in Italy first noticed a pattern in March 2020, when several covid patients developed Guillain-Barré syndrome, in which the immune systems attacks nerves throughout the body, causing muscle weakness or paralysis.
As the pandemic has surged around the world, doctors have diagnosed patients with rare, immune-related bleeding disorders. Other patients have developed the opposite problem, suffering blood clots that can lead to stroke.
All these conditions can be triggered by autoantibodies – rogue antibodies that target the patient's own proteins and cells.'
❂
✒ 2020
📖 (21 Dec 2020 ~ Frontiers in Immunology) Akt-Fas to Quell Aberrant T Cell Differentiation and Apoptosis in Covid-19 ➤
❂
📖 (18 Nov 2020 ~ Science / Translational Medicine) Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19 ➤
❂
📖 (17 Nov 2020 ~ Nature) Immune suppression in the early stage of COVID-19 disease ➤
❂
❊ 📖 (29 Oct 2020 ~ The Journal of Clinical Investigation) Sustained cellular immune dysregulation in individuals recovering from SARS-CoV-2 infection ➤
❂
❊ 📖 (28 Sept 2020 ~ Nature / Scientific Reports) Immune dysfunction following COVID-19, especially in severe patients ➤
❂
📖 (24 Sep 2020 ~ Science) Autoantibodies against type I IFNs in patients with life-threatening COVID-19 ➤
❂
📖 (17 Sep 2020 ~ Cell) Severe COVID-19 Is Marked by a Dysregulated Myeloid Cell Compartment ➤
❂
📖 (16 Sep 2020 ~ The Scientist) The Immune Hallmarks of Severe COVID-19 ➤
➲ 'Researchers are trying to make sense of immune systems gone haywire and develop biomarkers to predict who will become the sickest from a coronavirus infection.'
“Perhaps severe COVID-19 isn't a purely inflammatory disease, but rather a dangerous loop of ineffective human immune responses and continuous tissue inflammation.”
❂
📖 (16 July 2020 ~ Pre-print) AIDS and COVID-19 are two diseases separated by a common lymphocytopenia ➤
❂
📖 (29 June 2020 ~ PNAS) Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation ➤
❂
📖 20 Apr 2021 ~ Nature: Cell Death & Differentiation) SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination ➤
❂
❊ 📖 (1 May 2020 ~ Frontiers in Immunology) Reduction and Functional Exhaustion of T Cells in Patients With Coronavirus Disease 2019 (COVID-19) ➤
❂
Acknowledgement
My sincere thanks to Andrew Ewing of The World Health Network for helping to compile this list.
❂