‘These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens.’
📖
(2 Apr 2025 ~ CIDRAP)
‘COVID-19 may put patients at risk for other infections for at least 1 year’.
© 2025
S. Soucheray
/
CIDRAP.
❦
Scientific Media Article ~
‘COVID-19 may put patients at risk for other infections for at least 1 year’
By
Stephanie Soucheray
/
CIDRAP (2 Apr 2025)
‘In a study yesterday in
The Lancet Infectious Diseases, its authors describe how a positive test for COVID-19 is associated with increased rates of diagnosis of various non–SARS-CoV-2 infections in the 12 months following an acute SARS-CoV-2 infection, even if the initial infection is mild to moderate.
They also found that patients hospitalized for COVID-19 infections were at greater risk for other infections in the year after illness, compared to patients who were hospitalized for influenza.
❦
Almost 50% higher rate of non-COVID respiratory infections
Compared with the test-negative control group, participants with a positive COVID-19 test who were not admitted had significantly increased rates of outpatient diagnosis of bacterial, fungal, and viral infectious illnesses (increased risk of 17%), outpatient respiratory infections (increased risk of 46%), and admission to hospital for infectious illnesses (increased risk of 41%), including for sepsis and respiratory infections.
Overall, non-hospitalized COVID patients had higher rates in 32% of the 65 laboratory-based outcomes compared to those who tested negative for SARS-CoV-2.
That rate jumped in hospitalized COVID-19 patients, who had higher rates of positive results in 71% of the examined laboratory tests, after accounting for multiple comparisons with the COVID-negative cohort.
❦
COVID may alter immune function
To further analyze the association between COVID-19 and subsequent infections, the authors compared people admitted to the hospital for seasonal influenza (3,293) and those admitted for COVID-19 (12,450) in the VA database, and found that COVID patients had higher rates of admission to hospital for infectious illnesses (increased risk of 24%), admission to hospital for sepsis (increased risk of 35%), and in-hospital use of antimicrobials (increased risk of 23%).
“These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens,” Chodick writes in a
Lancet Comment on the study.
“The evidence suggests effects extending beyond the acute phase of infection, affecting even mild cases.”’
❂
📖 (2 Apr 2025 ~ CIDRAP)
COVID-19 may put patients at risk for other infections for at least 1 year ➤
© 2025
Stephanie Soucheray
/
CIDRAP.
📖
(1 Apr 2025 ~ The Lancet: Infectious Diseases)
‘Rates of infection with other pathogens after a positive COVID-19 test versus a negative test in US veterans (November 2021 to December 2023): a retrospective cohort study’.
© 2025
Cai
et al
/
The Lancet: Infectious Diseases.
❦
Study ~
‘Rates of infection with other pathogens after a positive COVID-19 test versus a negative test in US veterans (November 2021 to December 2023): a retrospective cohort study’
By
Cai et al
/
The Lancet: Infectious Diseases (1 Apr 2025)
‘In the 12 months of follow-up, compared with participants who had a negative test for COVID-19, people with COVID-19 who did
not require admission to hospital during the
acute phase of infection had
increased test positivity
rates for
bacterial infections (in blood, urine, and respiratory cultures) and
viral diseases (including
Epstein–Barr virus,
herpes simplex virus reactivation, and
respiratory viral infections).
People who were positive for COVID-19 and
admitted to
hospital also had
increased rates of
bacterial infections in blood, respiratory, and urine biospecimens, and
viral infections in blood and respiratory biospecimens.
Analyses of pre-specified outcomes showed that, compared with the test-negative control group, participants with a
positive COVID-19 test who were
not admitted to
hospital had
significantly increased rates of
outpatient diagnosis of
infectious illnesses (increased risk of
17%), including
bacterial,
fungal, and
viral infections;
outpatient respiratory infections (increased risk of
46%); and
admission to hospital for
infectious illnesses (increased risk of
41%), including for
sepsis and
respiratory infections; the rates of pre-specified outcomes were generally higher among those who were admitted to hospital for COVID-19 during the acute phase.
❦ COVID-19 vs. seasonal influenza
Compared with
people
admitted to hospital for
seasonal influenza, those admitted for
COVID-19 had
higher rates of admission to hospital for
infectious illnesses (increased risk of
24%), admission to hospital for
sepsis (increased risk of
35%), and
in-hospital use of antimicrobials (increased risk of
23%).’
❂
📖 (1 Apr 2025 ~ The Lancet: Infectious Diseases)
Rates of infection with other pathogens after a positive COVID-19 test versus a negative test in US veterans (November 2021 to December 2023): a retrospective cohort study ➤
© 2025
Cai
et al
/
The Lancet: Infectious Diseases.
📖
(1 Apr 2025 ~ The Lancet: Infectious Diseases ~ Comment)
‘Long-term infectious sequelae after SARS-CoV-2 infection should be considered in mild cases too’.
© 2025
Gabriel Chodick
/
The Lancet: Infectious Diseases ~ Comment.
❦
Comment ~
‘Long-term infectious sequelae after SARS-CoV-2 infection should be considered in mild cases too’
By
Gabriel Chodick
/
The Lancet: Infectious Diseases ~ Comment (1 Apr 2025)
❦
‘Cai and colleagues contribute important insights into a previously under-explored consequence: the
elevated rates of subsequent
infections following SARS-CoV-2 infection, including in people who had
not been admitted to
hospital for COVID-19 or
developed post-COVID-19-condition (also known as long COVID).
To establish whether these increased infection rates were unique to SARS-CoV-2, Cai and colleagues conducted comparative analyses with patients who were admitted to hospital for influenza.
Patients
admitted to hospital for
COVID-19 showed
higher rates of
all-cause admissions to hospital and
infectious illness-related hospitalisations, including
sepsis and
positive urine and
blood cultures, compared with patients admitted to hospital for influenza.
These findings complement a previous VA cohort study from the same group, which showed
51% greater all-cause mortality hazard in the
COVID-19 group
versus the
influenza group.
A
key advancement of Cai and colleagues’ study is the identification of
increased infection rates among patients who were
not admitted
to hospital [for COVID-19].
‘While previous research has primarily shown elevated rates of infection in patients with long-COVID, or in those requiring admission to hospital, this analysis demonstrates
substantial increases in
infection rates even in those with
mild initial disease.’
This builds upon another analysis of VA healthcare data, which showed increased rates of various non-communicable conditions in patients with COVID-19 who were
not admitted to hospital, including
pulmonary diseases,
hyperglycemia,
diabetes,
kidney disease, and
gastrointestinal complications.
‘These findings have important implications for understanding the
potential impact of
COVID-19 on
long-term immune function and
susceptibility to
pathogens.
The evidence suggests
effects extending beyond the
acute phase of infection, affecting even
mild cases.’
This growing body of research on post-acute COVID-19 sequelae supports a
bi-directional relationship between
non-communicable diseases and
infectious diseases, resulting in
persistently increased risk of
adverse outcomes in the
months and
years after initial
SARS-CoV-2 infection.’
❂
📖 (1 Apr 2025 ~ The Lancet: Infectious Diseases ~ Comment)
Long-term infectious sequelae after SARS-CoV-2 infection should be considered in mild cases too ➤
© 2025
Gabriel Chodick
/
The Lancet: Infectious Diseases ~ Comment.
by C19.Life... et al
•
29 September 2025
‘The arrival of the Omicron variant marked a major shift, introducing numerous extra mutations in the spike gene compared with earlier variants. Before Omicron, natural infection provided strong and durable protection against reinfection, with minimal waning over time. However, during the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year.’
by C19.Life... et al
•
7 September 2025
‘Vaccine effectiveness against SARS-CoV-2 [COVID-19] infection declines markedly with time and Omicron variants.’ from ‘Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection and severe outcomes in adults’ by Zhou et al / European Respiratory Review (2024).
by Guo et al / The Lancet ~ Infectious Diseases
•
5 June 2025
‘Importantly, NB.1.8.1 shows a balanced profile of ACE2 binding and immune evasion, supporting its potential for future prevalence.’
by Zhang et al / The Lancet ~ Microbe
•
3 June 2025
‘Since late 2024, a potential third major evolutionary shift in SARS-CoV-2 evolution might be unfolding. In November 2024 and January 2025, a highly mutated descendant of the Omicron subvariant BA.3 was detected in South Africa.’
by David Putrino ❂ Sonya Buyting ~ Radio-Canada / Canadian Broadcasting Corporation
•
20 March 2025
CBC Radio-Canada interview with long COVID [PASC] researcher David Putrino from the Icahn School of Medicine at Mount Sinai in New York.
by Chemaitelly et al / Nature
•
5 February 2025
‘Before Omicron, natural infection provided strong and durable protection against reinfection, with minimal waning over time. However, during the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year.’
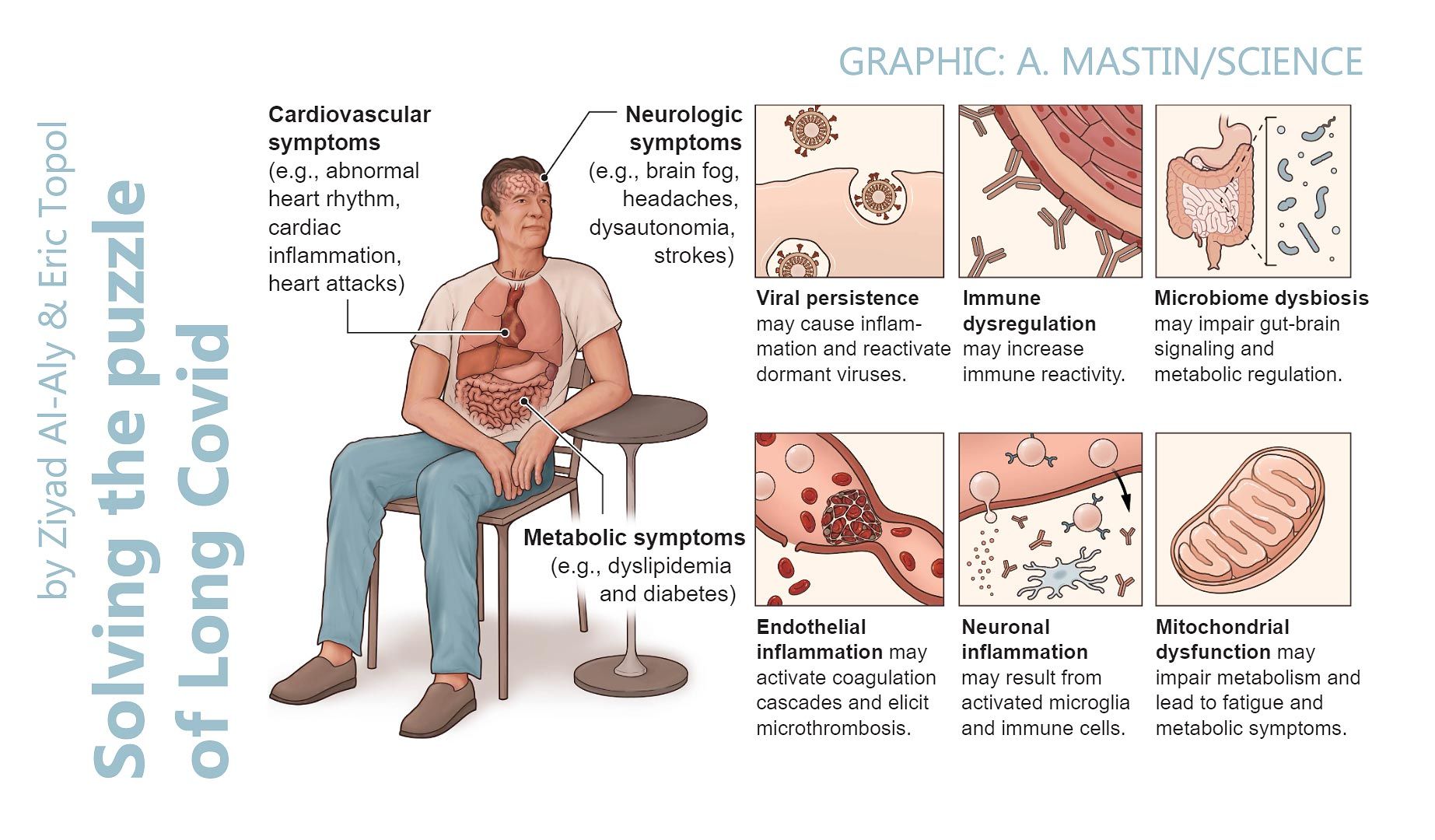
by Al-Aly & Topol / Science
•
22 February 2024
‘Reinfection, which is now the dominant type of SARS-CoV-2 infection, is not inconsequential; it can trigger de novo Long Covid or exacerbate its severity. Each reinfection contributes additional risk of Long Covid: cumulatively, two infections yield a higher risk of Long Covid than one infection, and three infections yield a higher risk than two infections.’
by Michael Merschel / American Heart Association
•
16 January 2024
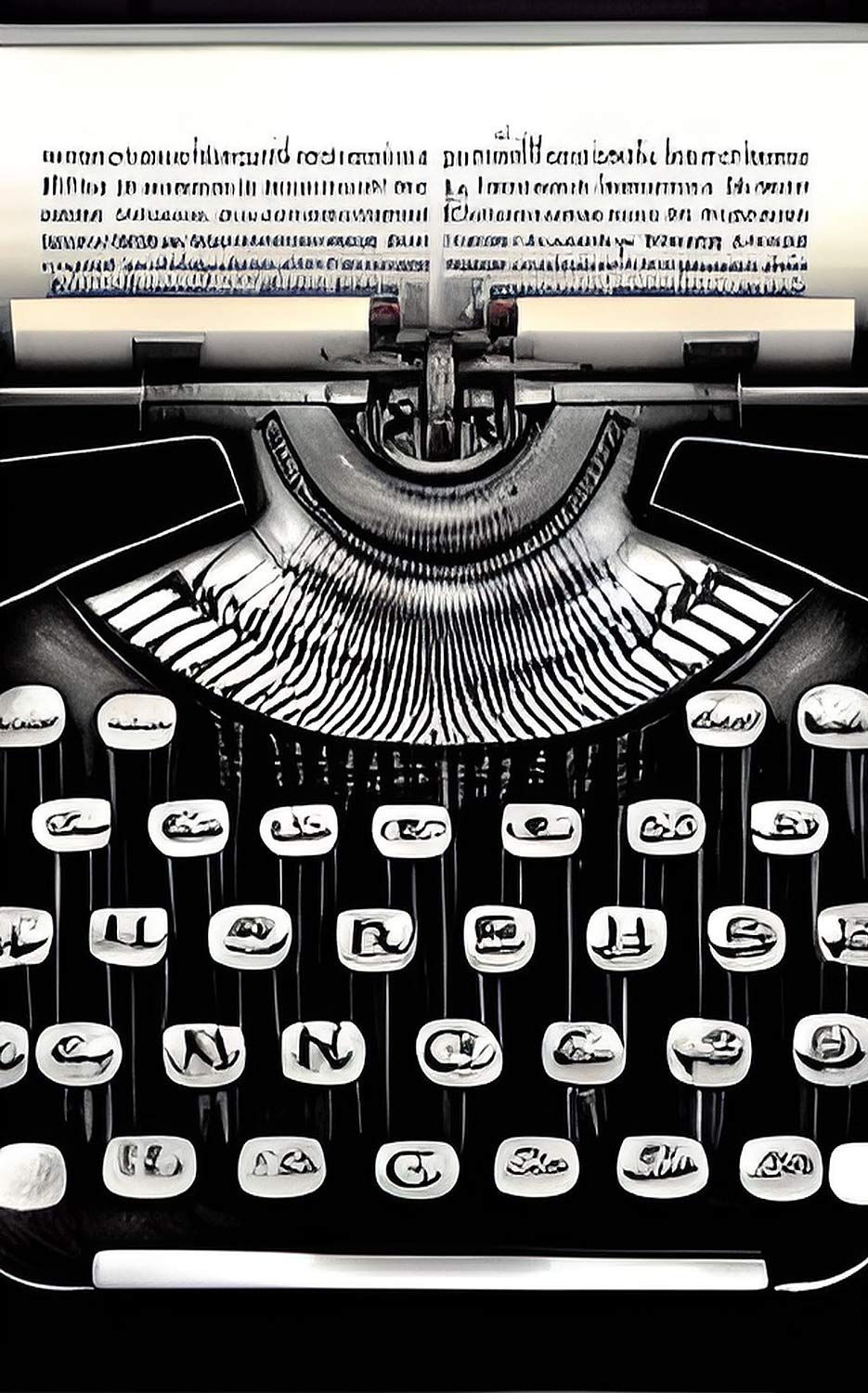
“I would argue that COVID-19 is not a disease of the lungs at all. It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system.”
by Conor Browne
•
28 November 2023
❦ “If you’re puzzled as to why governments and public health departments almost never mention even the possibility of SARS-CoV-2-induced immune dysregulation, it’s because to do so would be to admit the greatest mistake made in the history of modern health policy.” ❂ © 2023 Conor Browne ➲
by Cat in the Hat
•
22 November 2023
❦ Chris Whitty, from the Covid Inquiry: “The one situation... that you would ever aim to achieve herd immunity is by vaccination . That is the only situation that is a rational policy response.” And yet... the UK is no longer offering vaccines to the vast majority of its working-age population. According to the JCVI member Dr Adam Finn, the UK’s strategy going forward is that: “... most under 65’s will now end up boosting their immunity not through vaccination, but through catching Covid many times .” ➲ (24 Sep 2023 ~ BBC) What you need to know about Covid as new variant rises ➤ Let me translate: The stated aim is to get infected over and over and over again... to protect against being infected over and over and over again! How does this make any sense at all? The government has decided that it is not good “value for money” to actually give the boosters out – even for the age groups who have already had Covid vaccine doses purchased for them (for example, the 50-65 year olds) – so millions of doses [8.5 million] are now destined to be binned, rather than being used. ➲ ‘COVID VACCINE: COST EFFECTIVENESS ASSESSMENT. For the first time ever, the UK government has used a ‘bespoke, non-standard cost-effectiveness assessment’ to decide who would be eligible for the Covid booster this Autumn. In this thread, I explore how this assessment was undertaken…’ ➤ Meanwhile, in many other countries, the booster is open to anyone who wants it . No strict eligibility criteria. Just step forward and get protected. Let’s take a look at a few: 1. THE USA : Covid booster available to EVERYONE aged 6 months and older. The CDC (USA’s Centers for Disease Control ) recommends that everyone ages 6 months and upwards get the updated COVID-19 booster to protect against serious illness. The new vaccine targets the most common circulating variants, and should be available later this week. The full details are here ➤ . 2. CANADA : Covid booster available to EVERYONE aged 6 months and older. Full details are here ➤ . 3. FRANCE : Covid booster available to EVERYONE. Full details are here ➤ . 4. BELGIUM : Covid booster available to EVERYONE. Full details are here ➤ . 5. JAPAN : Covid booster available to EVERYONE aged 6 months and older. Full details are here ➤ . Why is the UK falling so far out of step with so many other countries on their Covid vaccine strategy? How can they justify binning millions of purchased vaccine doses when there are many people who would gladly take them? ➲ ‘So what’s going to happen to the millions of purchased doses which now won’t be used? Well, here’s the real kicker... it seems they’re destined for the bin. A number of alternative uses have been considered, but the conclusion is: “THESE DOSES HAVE NO FEASIBLE ALTERNATIVE USE”. ’ ➤ If the UK government won’t fund deployment of the Covid jab to EVERYONE (as so many other countries do), then why isn’t there at least an option to buy it privately? This model already exists with the flu jab – why is there not the same option for Covid? © 2023 Cat in the Hat ➲
by Dr. Adam Finn, Professor of Paediatrics, University of Bristol / Jim Reed, BBC
•
24 September 2023
❦ ‘The emergence of [new SARS-CoV-2 Variant of Interest] BA.2.86 meant a decision was made to bring forward the autumn Covid booster to better protect the most vulnerable this winter. But the new jabs are only available to people over 65 years old – it was the over-50s last year – and those with certain health conditions. That is a tactical decision , says Dr. Adam Finn, Professor of Paediatrics at the University of Bristol. He explained: “When younger people who’ve already had infections and vaccines get Covid [again], they get a cold and a cough and might be off work for a few days. There’s no real value in investing a lot of time and effort immunising them again when there are so many other things for the Health Service to be doing.” [ ❦ Note : Can a 62-year-old be defined as a ‘ younger person ’? Yes, at a pinch, if Mr. Finn compares them to a 78-year-old. What age-group do these ‘ younger people ’ belong to who don’t need vaccinating, and who instead need to be continually reinfected with a highly pathogenic Biohazard-Level 3 virus? Could it be a 32-year-old man or woman hoping to have a baby ? Or the 0 to 19-year-olds , who are the academic professor’s strong suit? ] ‘The reality is then that most under-65s will now end up boosting their immunity not through vaccination , but through catching Covid many times . In general, Prof Finn says each new infection should feel milder with the length of time you are sick reduced [sic] . “Each time you catch it, your immunity gets stronger and broader ,” he adds. ’ ❂ [ Note : This is simply not true, and is staggeringly dangerous. ] ❂ 📖 (24 Sep 2023 ~ Jim Reed, Health Reporter / BBC online) What you need to know about Covid as new variant [BA.2.86] rises ➤ © 2023 BBC .
by Merck and Co.
•
16 September 2023
❦ ‘The most common causes of acquired lymphocytopenia include: ➲ Protein-energy undernutrition. ➲ HIV infection. ➲ COVID-19 . ➲ Certain other viral infections. Patients with HIV infection routinely have lymphocytopenia, which arises from destruction of CD4+ T cells infected with the HIV virus. Patients with COVID-19 also frequently have lymphocytopenia ( 35% to 83% of patients ) . Lower lymphocyte counts portend a poor prognosis and an increased likelihood of requiring ICU admission and of dying from the disease. The cause of the lymphocytopenia is not completely understood, but COVID-19 can directly infect lymphocytes, and a cytokine-related apoptosis of the cells is likely. ➲ Lymphocytopenia is most often due to AIDS , and recently COVID-19 , or undernutrition, but it also may be inherited or caused by various infections, drugs, or autoimmune disorders. ➲ Patients have recurrent viral , bacterial , fungal , or parasitic infections .’ ❂ 📖 (Accessed 16 Sep 2023 ~ Merck & Co.) Entry for 'Lymphocytopenia' in Merck Manual ➤ © 2023 Merck & Co .
by Dr. Noor Bari, Emergency Medicine
•
27 August 2023
❦ “If y’all are busy weakening your immune systems with one virus, let me assure you that there are packs of other pathogens out there waiting to chew on the leftovers.”
by Altmann et al / Nature
•
11 July 2023
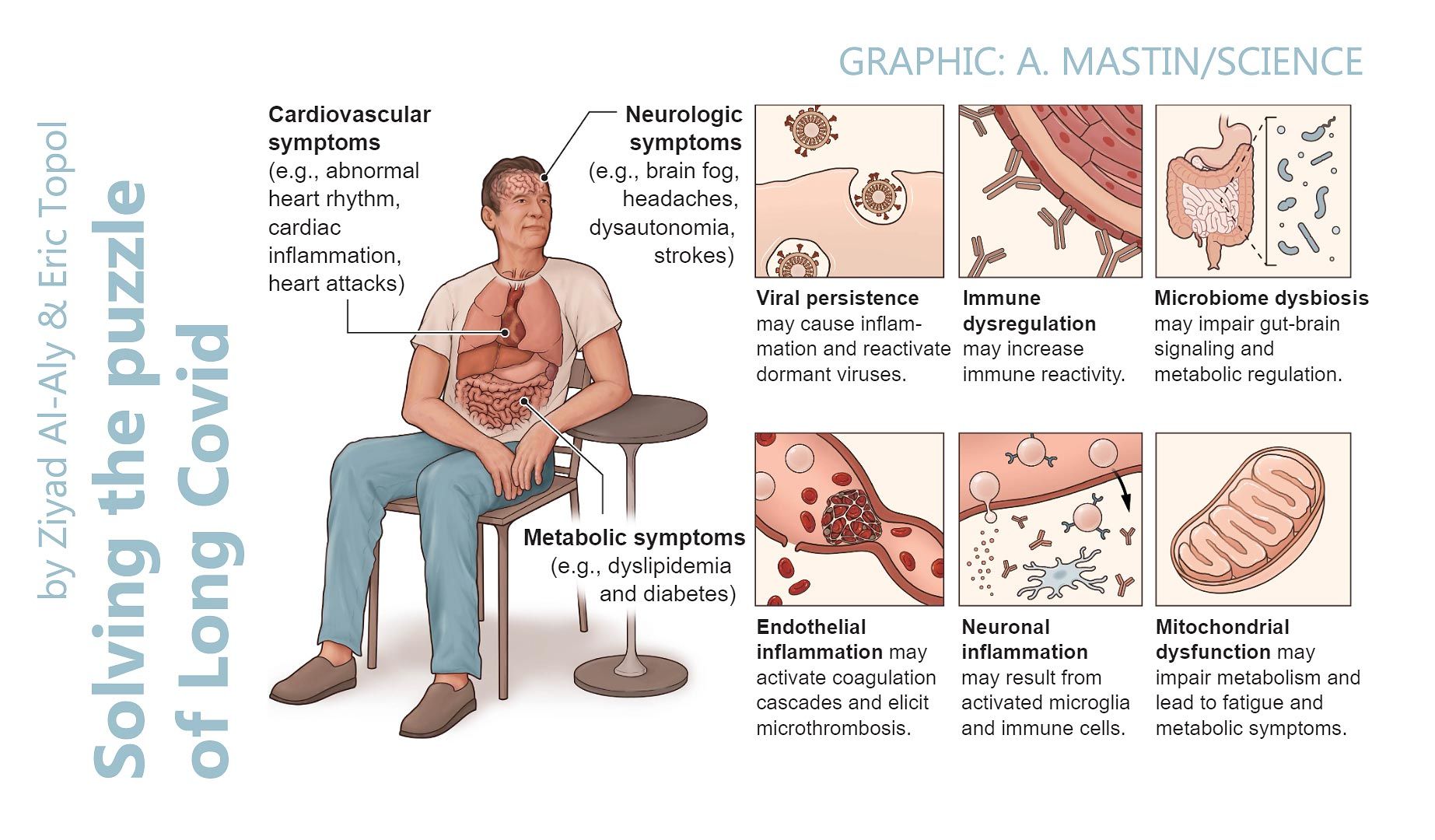
❦ ‘Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new healthcare challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with Long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein-Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. The oncoming burden of Long COVID faced by patients, healthcare providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it.’ ❂ 📖 (11 July 2023 ~ Nature Reviews: Immunology) The immunology of long COVID ➤ © 2023 Altmann et al / Nature.
by The John Snow Project
•
5 May 2023
❦ Prior to 2020, there were four endemic human coronaviruses – OC43, NL-63, 229E, and HKU1 – which were known to cause 10 to 15 percent of common colds – or the ‘Common Cold Coronaviruses’ (CCCs). From at least the 1970s, we’ve known that infection with these coronaviruses does not lead to lasting protection from reinfection – this is textbook knowledge. CCCs are not just colds – they can cause severe pneumonias, and exhibit a risk profile very similar to SARS-CoV-2 with age. If reinfection really did strengthen immunity against CCCs, then older people would be the least affected – because they would have been regularly infected with diverse variants of these viruses in their past. But that is not the case – and SARS-CoV-2 is not a CCC. SARS-CoV-2 has a wide array of accessory proteins that silence and disrupt our normal immune responses. As we get older, our immune systems start to lose their effectiveness – and we become more susceptible to disease. This process is called immunosenescence . Repeated exposure to a virus like SARS-CoV-2 is fast-tracking more people into immunosenescence at ever-earlier ages, with potentially serious repercussions for their health and longevity. SARS-CoV-2 is a particularly nasty virus that can also trigger the hyperactivation of our own immune systems to cause severe disease. Infection by SARS-CoV-2 has been shown to lead to an increase in autoantibodies and autoimmune disease. Approximately 25 percent of people who develop an autoimmune disease will experience multiple autoimmune syndrome, and will risk a cascade of autoimmune conditions. SARS-CoV-2, like its 2002 predecessor SARS-CoV-1, is both a respiratory and a systemic virus, with an extremely broad cell-type and tissue-tropism covering nearly the whole body. Its ability to infect and do damage to lungs, hearts, kidneys, cardiovascular systems and brains is particularly well-documented. If each subsequent infection results in additional internal organ and immune-system damage, then at some point the damage accumulated – together with the accelerated immune-system aging and normal aging processes – can reasonably be expected to outweigh the protective benefits of immunity developed from previous infections. SARS-CoV-2 reinfects more frequently than influenza or the common cold, infects a wider range of organs, does more damage and seems capable of persisting in a range of organs. So if SARS-CoV-2 behaves like a textbook virus – but does more damage more quickly and more regularly – at what point does the body reach its tipping point? ❂ There are two versions of this article: a 7-minute read in simplified language ; and the full editorial version complete with references, which is an 18-minute-read and aimed towards the medical and scientific communities . ❦ 7-minute primer ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❦ Full 18-minute editorial ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❂ 📖 (5 May 2023 ~ The John Snow Project) SARS-CoV-2 and "Textbook" Immunity ➤ © 2023 The John Snow Project.
by Negm et al / BMC Infectious Diseases
•
23 April 2023
❦ Critically ill COVID-19 patients are highly susceptible to opportunistic fungal infection due to many factors, including virus-induced immune dysregulation , host-related comorbidities, overuse and misuse of antibiotics or corticosteroids, immune modulator drugs, and the emergencies caused by the pandemic. Fungal coinfection is a common complication of critically ill COVID-19 patients admitted to the ICU. Candidiasis , aspergillosis , and mucormycosis are the most common COVID-19-associated fungal infections and have a great impact on mortality rates . ❂ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ © 2023 Negm et al / BMC Infectious Diseases.
by Sayyadi et al / Annals of Hematology
•
19 April 2023
❦ ‘COVID-19 patients have a hypercoagulability state, and thrombosis is a life-threatening complication of them.’ ✻ Hypercoagulability , also known as thrombophilia , is a condition in which there is an abnormally increased tendency towards blood clotting . ‘From the early days of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) outbreak to the present, clinical and basic studies have indicated that coronavirus disease 2019 (COVID-19) may be associated with coagulopathy ( CAC ), which is involved in its related morbidity and mortality. Deep vein thrombosis ( DVT ) and pulmonary embolism ( PE ) are common in COVID-19 patients and are remarkably high in the intensive care unit (ICU)–admitted patients. CAC can lead to the formation of circulating microthrombi and macrothrombi which can involve multiple sites, including the lungs , brain , heart , and visceral organs like kidneys and spleen . There is a close relationship between the immune system and coagulation. The components of the hemostatic system play a role in the body’s immunity, and the activation of the immune system strongly influences the hemostatic system. Abnormal activation of the immune system may promote the growth of pathologies associated with thrombosis. COVID-19 is accompanied by an immune-cell hyperactivation and excessive production of proinflammatory cytokines , known as “ cytokine storm ”. CAC is theorized to result from dysregulated interactions between the immune and coagulation systems .’ ❂ 📖 (19 Apr 2023 ~ Annals of Hematology) Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement ➤ © 2023 Annals of Hematology .
by Chen et al / Journal of Medical Virology
•
18 April 2023
❦ 'The risk of herpes zoster (HZ) [ shingles ] remained significantly higher [ +60% ] in patients with COVID-19, compared with those without COVID-19. The higher risk of HZ in the COVID-19 cohort compared with that in the non-COVID-19 cohort remained consistent across subgroup analyses regardless of vaccine status, age, or sex. The risk of HZ within a 12-month follow-up period was significantly higher in patients who had recovered from COVID-19 compared with that in the control group.' ❂ 📖 (18 Apr 2023 ~ Journal of Medical Virology) Long-term risk of herpes zoster following COVID-19: A retrospective cohort study of 2 442 686 patients ➤ © 2023 Journal of Medical Virology.
by Sharma & Jagadeesh / Nature Reviews: Rheumatology
•
12 April 2023
❦ The full picture of post-COVID-19 autoimmune diseases and their prevalence is lacking despite numerous case reports and small series. Two studies that use large cohorts now highlight that SARS-CoV-2 infection is linked to a substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases . The reports by Chang et al and Tesch et al provide a comprehensive overview of diverse new-onset autoimmune conditions after COVID-19. In addition, an earlier preprint of a retrospective matched cohort analysis using data from the Clinical Practice Research Datalink Aurum database of 458,147 SARS-CoV-2-infected and 1,818,929 uninfected adults across England between 31 January 2020 and 30 June 2021 reported that the incidence of type 1 diabetes mellitus , inflammatory bowel disease and psoriasis are significantly associated with SARS-CoV-2 infection. Some of the earliest evidence that SARS-CoV-2 infection leads to dysregulated immune responses came from paediatric patients who presented with multisystem inflammatory syndrome in children (MIS-C) , which, as the name indicates, involves diffuse organ system involvement and a clinical spectrum that overlaps with other hyperinflammatory syndromes , such as Kawasaki disease , toxic-shock syndrome , and macrophage activation syndrome . Since the start of the pandemic, many researchers have also reported isolated cases of adults with various post-COVID-19 autoimmune conditions. ❂ 📖 (12 Apr 2023 ~ Nature Reviews: Rheumatology) High risk of autoimmune diseases after COVID-19 ➤ © 2023 Sharma & Jagadeesh / Nature.
by Dr. Kevin Kavanagh, MD / Infection Control Today
•
31 March 2023
‘We are entering a phase of long COVID and chronic disability.’ ❂ ❦ ‘As the numbers of hospitalizations and deaths are dropping, many individuals declare the pandemic all but over, comforted by the belief that infections are mild and less dangerous than the seasonal flu. However, the scientific literature these last few weeks has been filled with deeply concerning reports. We are entering a phase of long COVID and chronic disability. The number of COVID-19 cases in the United States is unknown since our case reporting system has become unreliable and substantially undercounts cases. In England, as of the week ending March 7, 2023, 1 in 40 people is positive for COVID-19 , and reinfections are frequently occurring. It is estimated that as of November 9, 2022, 94% of the U.S. population has been infected by SARS-CoV-2 , and 65% of the United States population has been infected multiple times . The odds of self-reported long COVID were 28% less after the second infection. Unfortunately, the damage of long COVID from a second infection adds to the first . One of the most concerning long-term effects of COVID-19 is immune dysfunction or hypofunction . Confirmatory research was reported this week, and summarized in a National Institute of Health news release which stated: ‘… findings suggest that SARS-CoV-2 infection damages the CD8⁺ T cell response , an effect akin to that observed in earlier studies showing long-term damage to the immune system after infection with viruses such as hepatitis C or HIV .’ The authors conclude that this dysfunction causes lasting damage and may ‘contribute to long COVID, perhaps rendering patients unable to respond robustly to subsequent infections by SARS-CoV-2 variants or other pathogens .’ * * 📖 (20 Mar 2023 ~ National Institutes for Health) SARS-CoV-2 infection weakens immune-cell response to vaccination ➤ These findings mirror those reported by Files et al who state: ‘Overall, expression of these activation and exhaustion markers indicated more severe immune dysregulation of CD8 ⁺ T cells in the hospitalized group.’ And they found that ‘ CD8⁺ T cell expression of exhaustion markers increased in non-hospitalized individuals over time ’. * * 📖 (4 Jan 2021 ~ Journal of Clinical Investigation) Sustained cellular immune dysregulation in individuals recovering from SARS-CoV-2 infection ➤ The authors’ finding of damage to the immune system “akin” to HIV is very concerning, as is the amplification of this result in the NIH news release. Infection Control Today previously reported that the probable cause of the surges in infections we are seeing is an immune dysfunction caused by COVID-19 . With minimal public health interventions, Sweden also experienced surges in respiratory syncytial virus (RSV) cases. Most recently, Sweden has undergone a significant surge in seasonal flu, with reports from the Public Health Agency of Sweden of unusually severe cases. These [Swedish influenza] cases have occurred in ‘... people under the age of 18 without underlying disease or condition, and have been very seriously ill with complications such as myocarditis or encephalitis.’ Other diseases are also rising , exemplified by reports of record-high severe Streptococcal infections and Candida auris . These spikes in infections caused by multiple pathogens are associated with the SARS-CoV-2 pandemic and the mounting evidence of post-COVID-19 immune dysfunction. Vaccinations can not only reduce the incidence of severe disease, but can also help to prevent long COVID, reducing the incidence by 30% to 40%. However, we have expressed concern regarding the bivalent booster’s effectiveness, and reported a rapid waning of booster-induced immunity in the elderly. [See Footnote.] Recently, researchers from the United States found that the relative bivalent booster effectiveness at 5 to 7 months in preventing hospitalizations relative to monovalent vaccine dosages (2, 3, or 4) was 42% and 59% compared to no vaccination. Using the third vaccine dose as a baseline, the UK Health Security Agency found that an additional (fourth) vaccine dosage had effectiveness against hospitalizations at 10 weeks of only 50% .’ Source: 📖 (21 Mar 2023 ~ Infection Control Today) COVID-19: Study Suggests Long-term Damage to Immune System ➤ ❂ Footnote: On waning vaccine effectiveness * ‘Vaccine effectiveness is an important point. Although much of the younger population received a get-out-of-hospital free card for the latest variant, senior citizens were in its crosshairs. During the last 6 months (since May of 2022), those over the age of 75 had a higher rate of hospitalizations than in the Delta surge; those between the ages of 65 and 75 had approximately the same. Both age groups continue to be at high risk for death and disability. However, data showed that for those 65 years of age and older, the monovalent vaccine’s (2 or more doses) effectiveness for preventing hospitalizations fell to 28% in less than a year. Results were worse for those individuals under 65 years – only 19%.’ * 📖 (24 Feb 2023 ~ Infection Control Today) How Soon Is Another Booster Needed? Durability of Vaccine-Induced Immunity ➤ ❂ © 2023 Infection Control Today . ➲
by Dr. Noor Bari, Emergency Medicine
•
20 February 2023
❦ “I’m vaguely following the chatter on the comparisons of COVID with HIV. I’ve never been a fan of this, because there are so many unanswered questions. One thing I am sure of. Research shows the immune system does get damaged. It does. Which bits? How much? Recovery? What opportunistic infections? Impact on global disease patterns? Impact on animal disease patterns (ecology and food-chain threats)? All questions that will be answered over time. No-one should be surprised by this. It should not be even vaguely controversial. Plenty of viruses damage the immune system . We will find out exactly the extent of the nature of COVID on this aspect of health. Another thing I can say with some certainty. Your chances of recovery from a depressed post-viral immune system will not be improved by further [SARS-CoV-2] infections. I can see a lot of people directly comparing COVID with HIV. Rest assured. I am concerned. I just don’t find that particular comparison helpful. As many have already pointed out, there are significant differences too. You don’t walk into the supermarket and catch a new strain of HIV starting a whole new acute infection every 6-8 months, for example. But there are also signs that some immune cells are recovering many months after infection too – then again, there are probably reservoirs in the body that could potentially continue to mutate, and then cause other pathology down the line – as some animal coronaviruses do. I think COVID is quite an interesting and horrible disease. I expect we will see what repeated infections really do as time goes on. Excess deaths are already through the roof. One last attempt to clarify. Trying to make COVID into either a cold, or HIV, and ending up with “half-way between” – when in reality COVID is doing 100% COVID, which is turning out to be really, really bad in its own right… and it’s airborne… and we are catching it all the time. That’s the part I find frustrating with this comparison. SARS is a dangerous, dangerous disease. It always has been. Both of them [SARS-1 and SARS-2] . Yes, there are threads of similarities, and we can use our wealth of knowledge to extrapolate possible outcomes, and test treatments… But SARS is not half-way to anything. It is, in itself, a giant problem.”
by Rosichini et al / Journal of Allergy and Clinical Immunology
•
7 February 2023
❦ Lymphopenia , particularly when restricted to the T-cell compartment, has been described as one of the major clinical hallmarks in patients with coronavirus disease 2019 ( COVID-19 ) and proposed as an indicator of disease severity. Although several mechanisms fostering COVID-19-related lymphopenia have been described, including cell apoptosis and tissue homing, the underlying causes of the decline in T-cell count and function are still not completely understood. Patients with COVID-19 had reduced thymic function that was inversely associated with the severity of the disease. Our data demonstrate that the human thymus is a target of SARS-CoV-2 and thymic function is altered following infection . Note: Lymphopenia (also called lymphocytopenia) is a disorder in which your blood doesn't have enough white blood cells called lymphocytes. Lymphocytes play a protective role in your immune system. ❂ 📖 (7 Feb 2023 ~ Journal of Allergy and Clinical Immunology) SARS-CoV-2 infection of thymus induces loss of function that correlates with disease severity ➤ © 2023 Rosichini e t al / Journal of Allergy and Clinical Immunology.
by Emily Henderson ~ Medical Life Sciences / Tri Phan et al ~ Clinical Immunology
•
26 January 2023
❦ ‘Children have largely avoided severe COVID-19 symptoms because they have a strong initial ‘innate’ immune reaction that quickly defeats the virus. But unlike those of adults, children’s immune systems don’t remember the virus and don’t adapt, so when they’re next exposed to SARS-CoV-2, their body still treats it as a new threat. “Because children haven’t been exposed to many viruses, their immune system is still ‘naive’. And because they don't develop memory T cells, they are at risk of getting sick when they become reinfected. With each new infectious episode as they get older, there is a risk of their T cells becoming ‘exhausted’ and ineffective, like the T cells in older people. The price that children pay for being so good at getting rid of the virus in the first place is that they don’t have the opportunity to develop ‘adaptive’ memory to protect them the second time they are exposed to the virus,” says Professor Tri Phan.’ ❂ 📖 (26 Jan 2023 ~ Medical Life Sciences) Children's immune systems do not develop 'adaptive' memory to protect against second-time SARS-CoV-2 infection ➤ 📖 (January 2023 ~ Clinical Immunology) Tracking the clonal dynamics of SARS-CoV-2-specific T cells in children and adults with mild/asymptomatic COVID-19 ➤ © 2023 Emily Henderson / Medical Life Sciences.
by Emily Henderson / News Medical Life Sciences
•
12 January 2023
❦ Fungi such as Aspergillus are so common in our surroundings that we breathe in hundreds to thousands of spores every day. In healthy people, fungi typically pose no threat, but they can cause deadly infections in those with compromised immune systems. However, it is increasingly recognized that viral infections such as influenza or SARS-CoV-2 can increase the risk of invasive Aspergillus infections even in healthy people. ❂ 📖 (12 Jan 2023 ~ News-Medical.Net) New insights into deadly fungal invasion in people with compromised immune systems ➤ © 2023 Emily Henderson / News Medical Life Sciences.
by Terry Pender / Waterloo Region Record
•
20 December 2022
❦ Evolving research says COVID leaves many people at heightened risk for other infections. SARS-CoV-2 depletes the body’s supply of T-cells, * leaving young and old alike vulnerable to secondary infections. * (T-cells are the ‘front-line soldiers’ of the immune system, and the number of T-cells typically increases when the body is fighting off an infection.) “Individuals who are infected with COVID have many fewer T-cells – that’s a problem for us, because T-cells are a really important part of our immune system that helps defend us against infection.” But at least three studies show ✢ that COVID kills off a significant number of the body’s T-cells – so even when someone recovers from COVID, they are at a heightened risk for other viral, bacterial and fungal infections. “With the loss of these T-cells, we are now more vulnerable to all of these other infections, other viruses, other bacteria.” COVID-19 sparks what is called ‘programmed cell death’ among T-cells. Cells in the human body do this naturally as they age, but COVID-19 causes healthy T-cells to die that would otherwise be available to fight off infections. Many people who have had COVID brush it off, saying it was no worse than a bad case of the flu. What they don’t know is that they are more vulnerable to secondary infections that may cause them to seek help at a hospital emergency ward. ❂ ✢ 📖 (11 Jan 2023 ~ Nature Reviews / Immunology) Innate immune evasion strategies of SARS-CoV-2 ➤ 📖 (13 Jan 2023 ~ Preprint) Structure-based discovery of inhibitors of the SARS-CoV-2 Nsp14 N7-methyltransferase ➤ 📖 20 Apr 2021 ~ Nature / Cell Death & Differentiation) SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination ➤ ❂ 📖 (20 Dec 2022 ~ Waterloo Region Record) Immune systems seriously weakened by COVID ➤ © 2022 Terry Pender / Waterloo Region Record.
by Davitt et al / Best Practice & Research Clinical Haematology
•
6 December 2022
❦ While COVID-19 was originally characterized as hyperinflammatory in its pathophysiology, emerging evidence demonstrates the possibility of a strongly immunosuppressive phenotype in more critical disease states. While immune activation from neutrophils and complement may contribute to inflammatory damage in the lungs, decreased antiviral responses, dysregulated macrophages and dendritic cells, and severe lymphopenia contribute to a suppressed state in which viral replication and secondary infections are prone. ❂ 📖 (6 Dec 2022 ~ Best Practice & Research Clinical Haematology) COVID-19 disease and immune dysregulation ➤ © 2022 Davitt et al / Best Practice & Research Clinical Haematology.
by Dr. Noor Bari, Emergency Medicine
•
30 November 2022
❦ “Lymphopenia is present during and after some viral infections, and this also varies between individuals. It is very transient in most cases, and by that I mean a couple of weeks. The viruses that cause longer derangement are already known to be associated with long-term immune system derangement – including secondary infections, immune amnesia and cancers. COVID-19 lymphopenia has been recorded present for months. COVID-19 has been found to destroy (engulf in syncytia), directly infect, stimulate, and suppress a lot of white-cell function. Reinfections are frequent. Secondary infections/reactivations observed. It’s a huge worry. As a general rule, efforts are made to control/treat viruses that cause prolonged immune system derangement. COVID-19 is wildly exceptional in that we are ignoring it, pretending the lymphocytes bounce back like after a cold, and are frequently infecting people with it. We are also losing naive lymphocytes in large numbers due to superantigen stimulation. This is very different to transient suppression of peripheral blood lymphocytes due to cytokines or migration. This is another example of people making assumptions (huge and wrong), based on entirely dissimilar pathogens. It’s very important to look at what happens in similar situations, such as post-other-super-antigen-carrying infections. (Nothing good.) I could have saved my energy today and just let everyone play with a super antigen and find out… but sadly, the people finding out the hardest lessons are not the people deciding to play with it. So… here we are…”
by Dr. Noor Bari, Emergency Medicine
•
10 November 2022
❦ “This morning someone said to me: — “I just can’t shake this... first a chest infection, and now a urine infection...” Someone else I know (very close) has had three eye infections post-COVID. Another has had a deterioration in their fertility, as compared to their baseline pre- and post-COVID. Measured. It’s almost as if the stuff in the science papers is real. None of them have twigged that COVID might have toasted them yet either. They are all heading into this next wave with no idea how dangerous it might be to abuse their already struggling immune system like this. You know what’s coming next... Multi-drug-resistant bacteria. Many are already here, but this is going to get really out of control. Trying to treat infections in immunodeficient patients is a great way to make loads of drug-resistant bacteria and viruses.” ✾ 📖 (24 Sep 2025 ~ CIDRAP/University of Minnesota) Outpatient antibiotic use in COVID patients linked to 'downstream' antibiotic resistance ➤ 📖 (15 Jul 2025 ~ UKHSA: News story) UTIs [Urinary Tract Infections] cost NHS hospitals over £600m last year ➤ 📖 (26 Jun 2025 ~ Forbes) Cancer Patients Face Silent Crisis From Superbugs, New Research Shows ➤ 📖 (12 Dec 2024 ~ CIDRAP/University of Minnesota) Report describes spread of highly drug-resistant cholera strain ➤ 📖 (1 Nov 2024 ~ China CDC Weekly) Emergence of a New Sublineage of Candida auris Causing Nosocomial Transmissions - Beijing Municipality, China, March-September 2023 ➤ 📖 (17 May 2024 ~ CIDRAP/University of Minnesota) Global Meta-analysis estimates 43% rate of multidrug resistance in COVID patients ➤ 📖 (14 May 2024 ~ Journal of Infection) Global antimicrobial resistance and antibiotic use in COVID-19 patients within health facilities: A systematic review and meta-analysis of aggregated participant data ➤ 📖 (24 May 2023 ~ Current Microbiology) Interaction Between SARS-CoV-2 and Pathogenic Bacteria ➤ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ 📖 (29 Mar 2023 ~ Journal of Fungi) Fungal-Bacterial Co-Infections and Super-Infections among Hospitalized COVID-19 Patients: A Systematic Review ➤ 📖 (30 Sep 2021 ~ Business Insider) Drug-resistant infections in the US have risen sharply during the pandemic, and experts warn it's getting worse as COVID patients overwhelm hospital resources ➤
by Dr. Noor Bari, Emergency Medicine
•
30 October 2022
❦ “COVID-19 is fighting back by generally depressing the whole adaptive immune system. We are showing narrow resilience to COVID reinfections due to adapting – but we are becoming more vulnerable in general to infections of all kinds. ❦ Worst case scenario A single infection causes on-going and progressive immunodeficiency . ❦ Best case scenario A single infection causes temporary immunosuppression , and we suppress COVID transmission enough to allow recovery. ❦ Most likely scenario, medium-term Immunosuppression that becomes continuous and possibly progressive due to reinfections. Reduced immune function after a viral infection is not unusual. Many viruses do this. The concerning issue is the length and breadth of the immune system dysfunction, coupled with emerging evidence of other pathogens taking advantage .” ✾ ❦ Immunosuppression ~ Suppression of the immune system and its ability to fight infection. ❦ Immunodeficiency ~ A state in which the immune system’s ability to fight infectious diseases and cancer is compromised, or entirely absent.
by Dr. Lisa Iannattone, Assistant Professor of Dermatology
•
15 October 2022
❦ “Not catching a common virus for a year or two, or five, does not make you respond to it like an immunosuppressed person the next time you catch it. Avoiding pathogens doesn’t damage your immune system. On the other hand, there are many pathogens out there that are capable of damaging your immune system. Pathogens are foes, not friends.”
by Dr. Lisa Iannattone, Assistant Professor of Dermatology
•
1 October 2022
❦ “Immunity debt” is making the rounds again. So here’s my reminder that while there are viruses that are more severe if caught as a teen or adult (like polio or chickenpox), that isn’t the case for respiratory viruses . There’s a mortality benefit from first RSV and flu infections being delayed. So no, your toddler doesn’t need to catch all the viruses before the age of two to “build their immune system”. In fact, it’s the opposite: infants and young toddlers are more at risk of hospitalization and death from many respiratory viruses at their age than older children. You know how we’re asked not to give kids honey until they’re one? Or how Health Canada has a whole list of unsafe foods for kids under five? “ For many pathogens, kids are more susceptible to severe outcomes when they’re very young. ” And there is benefit to delaying exposure. This new (and very politically convenient) idea that it’s always best to catch pathogens very early in life “to build your immune system” can actually be quite dangerous when you take the time to think it all the way through. Stop blindly promoting “immunity debt” pseudoscience. Three years ago, I never would have believed that I’d one day see scientists and MDs [medical doctors] promoting the idea that it’s good for infants and young toddlers to be exposed to dangerous respiratory viruses like flu and RSV, instead of trying to delay those first infections – and yet here we are.”
by Hayley Muendlein / The Conversation
•
17 August 2022
❦ The 1918 influenza pandemic resulted in the loss of over 3% of the world’s population – at least 50 million people. But it wasn’t the flu virus that caused the majority of these deaths. An analysis of lung samples collected during that flu pandemic indicated that most of the deaths were likely due to bacterial pneumonia , which ran rampant in the absence of antibiotics. Even in more recent history, like the 1957 H2N2 and 2009 H1N1 flu pandemics , nearly 18% of patients with viral pneumonia had additional bacterial infections that increased their risk of death. And the COVID-19 pandemic is no different. ❂ 📖 (17 Aug 2022 ~ The Conversation) When COVID-19 or flu viruses kill, they often have an accomplice – bacterial infections ➤ © 2022 Hayley Muendlein / The Conversation.
by Dr. Noor Bari, Emergency Medicine
•
21 July 2022
❦ “So, we want to “live with the virus”. Is there any evidence of this occurring successfully anywhere? Yes! In bats... and it has taken 64 million years of evolution to get there. To “live with the virus”, bats have better host defences – they don’t overdo inflammation, and they can get rid of toxic compounds and deal with reactive oxygen species much better than humans. They literally live with the virus .
by Liz Szabo / KFF Health News
•
4 March 2021
❦ While all viruses find ways to evade the body’s defenses, a growing field of research suggests that the coronavirus unhinges the immune system more profoundly than previously realized. Some Covid survivors have developed serious autoimmune diseases, which occur when an overactive immune system attacks the patient, rather than the virus. Doctors in Italy first noticed a pattern in March 2020, when several Covid patients developed Guillain-Barré syndrome, in which the immune systems attacks nerves throughout the body, causing muscle weakness or paralysis. As the pandemic has surged around the world, doctors have diagnosed patients with rare, immune-related bleeding disorders. Other patients have developed the opposite problem, suffering blood clots that can lead to stroke. All these conditions can be triggered by autoantibodies – rogue antibodies that target the patient’s own proteins and cells. ❂ 📖 (4 Mar 2021 ~ KFF Health News) Coronavirus Deranges the Immune System in Complex and Deadly Ways ➤ © 2021 Liz Szabo / KFF Health News.
More... PASC (‘Long COVID’)
by C19.Life... et al
•
21 November 2025
‘Although COVID-19 was originally considered a respiratory illness, it is now well established that SARS-CoV-2 infection can have far-reaching impacts on the nervous system. Common neurological symptoms in Long COVID [PASC] include new-onset cognitive difficulties, dysautonomia, fatigue, and peripheral neuropathy.’ from ‘Neuroimmune pathophysiology of long COVID’ by Moen et al / Psychiatry and Clinical Neurosciences (2025).
by David Putrino ❂ Sonya Buyting ~ Radio-Canada / Canadian Broadcasting Corporation
•
20 March 2025
CBC Radio-Canada interview with long COVID [PASC] researcher David Putrino from the Icahn School of Medicine at Mount Sinai in New York.
by Jason Gale / Bloomberg UK
•
3 March 2025
‘For patients already battling Alzheimer’s disease, studies indicate that Covid can exacerbate brain inflammation, damage immune cells, and accelerate the disease. Even previously healthy older adults face an increased risk of cognitive impairment and new-onset dementia after infection. Mild Covid cases in younger adults have also been linked to brain issues affecting memory and thinking. ’
by C19.Life... et al
•
28 February 2025
‘But even people who had not been hospitalized had increased risks of many conditions, ranging from an 8% increase in the rate of heart attacks to a 247% increase in the rate of heart inflammation.’ Nature (2 Aug 2022) ‘Either symptomatic or asymptomatic SARS-CoV-2 infection is associated with increased risk of late cardiovascular outcomes and has causal effect on all-cause mortality in a late post-COVID-19 period.’ The American Journal of Cardiology (15 Sep 2023)
by Huang et al / BMC Medicine
•
6 February 2025
‘The proportions of PACS [PASC/Long Covid] patients experiencing chest pain, palpitation, and hypertension as sequelae were 22%, 18%, and 19% respectively.’
by News Medical Life Sciences ❂ Duff et al / Nature Medicine
•
2 February 2025
‘Scientists discover that even mild COVID-19 can alter brain proteins linked to Alzheimer’s disease, potentially increasing dementia risk. COVID-19-positive individuals exhibited lower cognitive test performance compared to controls – equivalent to almost two years of age-related cognitive decline. ’
by R. Peter et al / PLOS Medicine
•
23 January 2025
‘The predominant symptoms, often clustering together, remain fatigue, cognitive disturbance and chest symptoms, including breathlessness, with sleep disorder and anxiety as additional complaints. Many patients with persistent PCS [PASC/‘Long Covid’] show impaired executive functioning, reduced cognitive processing speed and reduced physical exercise capacity.’
by C19.Life
•
16 November 2024
❦ On that 700-day cough... It’s a new thing, but it’s only reserved for inside supermarkets and offices. And pharmacies and hospitals and care homes. Oh, and your living-room. But apart from that, it’s not exactly a deal-breaker. I mean, c’mon. They put up with way worse in the 1900s.
by Porter et al / The Lancet: Regional Health (Americas)
•
23 October 2024
❦ ‘In this population of healthy young adult US Marines with mostly either asymptomatic or mild acute COVID-19, one fourth reported physical , cognitive , or psychiatric long-term sequelae of infection. The Marines affected with PASC [Post-Acute Sequelae of COVID-19 / Post-COVID-19 Complications / ‘Long Covid’] showed evidence of long-term decrease in functional performance suggesting that SARS-CoV-2 infection may negatively affect health for a significant proportion of young adults .’ ❂ ‘Among the 899 participants, 88.8% had a SARS-CoV-2 infection. Almost a quarter (24.7%) of these individuals had at least one COVID-19 symptom that lasted for at least 4 weeks meeting the a priori definition of PASC established for this study. Among those with PASC, 10 had no acute SARS-CoV-2 symptoms after PCR-confirmed infection suggesting that PASC can occur among asymptomatic individuals. Many participants reported that lingering symptoms impaired their productivity at work, caused them to miss work, and/or limited their ability to perform normal duty/activities. Marines with PASC had significantly decreased physical fitness test scores up to approximately one year post-infection with a three-mile run time that averaged in the 65th percentile of the reference cohort. [ PASC was associated with a significantly increased 3-mile run time on the standard Marine fitness test. PASC participants ran 25.1 seconds slower than a pre-pandemic reference cohort composed of 22,612 Marine recruits from 2016 to 2019. A three-mile run evaluates aerobic exercise , overhead lifting of an ammunition can and pull-ups evaluate strength , and shooting a rifle evaluates fine-motor skills .] Scores for events evaluating upper body (pull-ups, crunches, and ammo-can lift) were not significantly reduced by PASC; however, overall physical fitness scores were reduced. ‘The poorer run times and overall scores among PASC participants are indicative of on-going functional effects.’ Standardized health-based assessments for somatization, depression, and anxiety further highlighted the detrimental health effects of PASC. Almost 10% of participants with PASC had PHQ-8 scores ≥10. Increased somatization * has been associated with increased stress, depression, and problems with emotions. * [ Somatization / Somatisation = Medical symptoms caused by psychological stress.] Additionally, PASC participants had higher GAD-7 scores suggesting increased anxiety in a population with unique inherent occupational stressors associated with higher rates of anxiety, depression, and post-traumatic stress disorder. ‘Increased severity of anxiety among those with PASC, combined with greater rates of mental health disorders in general, could portend an ominous combination and should be closely followed.’ Like others, we identified cardiopulmonary symptoms as some of the most prevalent. The high prevalence of symptoms like shortness of breath, difficulty breathing, cough, and fatigue is particularly notable when combined with decreased objective measures of aerobic performance such as running. These results suggest pathology in the cardiopulmonary system. In contrast we observed no reduction in scores assessing strength and marksmanship suggesting the lack of detectable pathology in the neuro-musculoskeletal system. We have previously found in this same cohort that SARS-CoV-2 infection causes prolonged dysregulation of immune cell epigenetic patterns like auto-immune diseases. Based on the reported PASC symptoms, the potential current and future public health implications in this population could be substantial. ‘Chronic health complications from PASC, especially in a young and previously healthy population with a long life expectancy, could decrease work productivity and increase healthcare costs.’ Significant changes in the Years-of-Life lived with a disability can disproportionally increase disability-adjusted life-years, and should be considered when allocating resources and designing policy.’ ❂ 📖 (23 Oct 2024 ~ The Lancet: Regional Health/America) Clinical and functional assessment of SARS-CoV-2 sequelae among young marines – a panel study ➤ © 2024 The Lancet .
by Dempsey et al / BMJ Journals ~ Occupational and Environmental Medicine
•
8 October 2024
‘This study included 5248 healthcare workers. While 33.6% reported prolonged COVID-19 symptoms consistent with PCS, only 7.4% reported a formal diagnosis of PCS. Fatigue, difficulty concentrating, insomnia, and anxiety or depression were the most common PCS [Post-COVID-19 Syndrome] symptoms. Baseline risk factors for reporting PCS included screening for common mental disorders, direct contact with COVID-19 patients, pre-existing respiratory illnesses, female sex and older age.’
by Al-Aly & Topol / Science
•
22 February 2024
‘Reinfection, which is now the dominant type of SARS-CoV-2 infection, is not inconsequential; it can trigger de novo Long Covid or exacerbate its severity. Each reinfection contributes additional risk of Long Covid: cumulatively, two infections yield a higher risk of Long Covid than one infection, and three infections yield a higher risk than two infections.’
by Greene et al / Nature: Neuroscience [Commentary by Danielle Beckman]
•
22 February 2024
❦ “This study confirms everything that I have seen in the microscope over the last few years. The authors of the study use a technique called dynamic contrast-enhanced magnetic resonance imaging ( DCE-MRI ), an imaging technique that can measure the density , integrity , and leakiness of tissue vasculature. Comparing all individuals with previous COVID infection to unaffected controls revealed decreased general brain volume in patients with ‘brain fog’ – along with significantly reduced cerebral white matter volume in both hemispheres in the recovered and ‘brain fog’ cohorts . Covid-19 induces brain-volume loss and leaky blood-brain barrier in some patients. How can this be more clear?” © 2024 Dr. Danielle Beckman, Neuroscientist (PhD Biological Chemistry) ➲ ❂ 📖 (22 Feb 2024 ~ Nature: Neuroscience) Blood–brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment ➤ ‘ Our data suggest that sustained systemic inflammation and persistent localized blood-brain barrier (BBB) dysfunction is a key feature of long COVID-associated brain fog. Patients with long COVID had elevated levels of IL-8, GFAP and TGFβ, with TGFβ specifically increased in the cohort with brain fog. GFAP is a robust marker of cerebrovascular damage and is elevated after repetitive head trauma, reflecting BBB disruption, as seen in contact sport athletes and in individuals with self-reported neurological symptoms in long COVID. Interestingly, TGFβ was strongly associated with BBB disruption and structural brain changes. ’ [Layperson overview] 📖 (February 2024 ~ Genetic Engineering and Biotechnology News) Leaky Blood Vessels in the Brain Linked to Brain Fog in Long COVID Patients ➤ [Related] 📖 (7 Feb 2022 ~ Nature: Cardiovascular Research) Blood–brain barrier link to human cognitive impairment and Alzheimer’s disease ➤ ❂
by Meng et al / The Lancet: eClinical Medicine
•
17 February 2024
❦ ‘The occurrences of respiratory disorders among patients who survived for 30 days after the COVID-19 diagnosis continued to rise consistently, including asthma , bronchiectasis , COPD , ILD , PVD * , and lung cancer . * COPD = Chronic obstructive pulmonary disease . ILD = Interstitial lung disease . PVD = Peripheral vascular disease . With the severity of the acute phase of COVID-19, the risk of all respiratory diseases increases progressively. Besides, during the 24-months follow-up, we observed an increasing trend in the risks of asthma and bronchiectasis over time, which indicates that long-term monitoring and meticulous follow-up of these patients is essential. These findings contribute to a more complete understanding of the impact of COVID-19 on the respiratory system and highlight the importance of prevention and early intervention of these respiratory sequelae of COVID-19. In this study, several key findings have been further identified. Firstly, our research demonstrates a significant association between COVID-19 and an increased long-term risk of developing various respiratory diseases. Secondly, we found that the risk of respiratory disease increases with severity in patients with COVID-19, indicating that it is necessary to pay attention to respiratory COVID-19 sequelae in patients, especially those hospitalized during the acute stage of infection. This is consistent with the findings of Lam et al., who found that the risk of some respiratory diseases (including chronic pulmonary disease, acute respiratory distress syndrome and ILD) increased with the severity of COVID-19. Notably, however, our study found that asthma and COPD remained evident even in the non-hospitalized population. This emphasizes that even in cases of mild COVID-19, the healthcare system should remain vigilant. Thirdly, we investigated differences in risk across time periods, as well as the long-term effects of COVID-19 on respiratory disease. During the 2-years follow-up period, the risks of COPD, ILD, PVD and lung cancer decreased, while risks of asthma and bronchiectasis increased. Fourthly, our study showed a significant increase of the long-term risk of developing asthma, COPD, ILD, and lung cancer diseases among individuals who suffered SARS-CoV-2 reinfection. This finding emphasizes the importance of preventing reinfection of COVID-19 in order to protect public health and reduce the potential burden of SARS-CoV-2 reinfection. Interestingly, vaccination appears to have a potentially worsening effect on asthma morbidity compared with other outcomes. This observation aligns with some previous studies that have suggested a possible induction of asthma onset or exacerbation by COVID-19 vaccination. It suggests that more care may be necessary for patients with asthma on taking the COVID vaccines. The underlying mechanisms associated with COVID and respiratory outcomes are not fully understood, but several hypotheses have been proposed. First, SARS-CoV-2 can persist in tissues (including the respiratory tract), as well as the circulating system for an extended period of time after the initial infection. This prolonged presence of the virus could directly contribute to long-term damage of the respiratory tissues, consequently leading to the development of various respiratory diseases. Second, it has been observed that SARS-CoV-2 infection can lead to prolonged immunological dysfunctions, including highly activated innate immune cells, a deficiency in naive T and B cells, and increased expression of interferons and other pro-inflammatory cytokines. These immune system abnormalities are closely associated with common chronic respiratory diseases – asthma, bronchiectasis, COPD, as well as the development of lung cancer. Next, SARS-CoV-2 itself has been shown to drive cross-reactive antibody responses, and a range of autoantibodies were found in patients with COVID-19. In conclusion, our research adds to the existing knowledge regarding the effects of COVID-19 on the respiratory system. Specifically, it shows that the risk of respiratory illness increases with the severity of infection and reinfection. Our findings emphasize the importance of providing extended care and attention to patients previously infected with SARS-CoV-2.’ ❂ 📖 (17 Feb 2024 ~ The Lancet: eClinical Medicine) Long-term risks of respiratory diseases in patients infected with SARS-CoV-2: a longitudinal, population-based cohort study ➤ © 2024 The Lancet: eClinical Medicine .
by Henry Madison
•
9 February 2024
❦ “Chronic disease is like the perfect medical crime. The cause is usually long gone by the time the disease manifests, and nobody links the two until it’s much too late for most.” ❂ © 2024 Henry Madison . ➲
by Dr. David Joffe PhD / FRACP (Respiratory Physician)
•
27 January 2024
❦ “It’s really not in the interest of the virus to kill us quickly. That’s why it has mutated to immune escape. That way it enters silently, and then eats you slowly whilst you’re still a spreading vector. Refrigerator trucks are long gone. That’s all the political class wanted. The unseen costs of CVD [cardiovascular disease] , DM [diabetes mellitus] , and both dementia and Parkinson’s Disease are the train coming down the tunnel. The economists are catching up. The actuaries are already there. Politicians and most people? Not yet...” ❂ © 2024 Dr. David Joffe PhD / FRACP (Respiratory Physician) ➲
by Scardua-Silva et al / Nature: Scientific Reports
•
19 January 2024
❦ ‘Although some studies have shown neuroimaging and neuropsychological alterations in post-COVID-19 patients, fewer combined neuroimaging and neuropsychology evaluations of individuals who presented a mild acute infection. Here we investigated cognitive dysfunction and brain changes in a group of mildly infected individuals. We conducted a cross-sectional study of 97 consecutive subjects ( median age of 41 years ) without current or history of psychiatric symptoms (including anxiety and depression) after a mild infection , with a median of 79 days (and mean of 97 days ) after diagnosis of COVID-19. We performed semi-structured interviews, neurological examinations, 3T-MRI scans, and neuropsychological assessments. The patients reported memory loss ( 36% ), fatigue ( 31% ) and headache ( 29% ). The quantitative analyses confirmed symptoms of fatigue ( 83% of participants), excessive somnolence ( 35% ), impaired phonemic verbal fluency ( 21% ), impaired verbal categorical fluency ( 13% ) and impaired logical memory immediate recall ( 16% ). Our group… presented higher rates of impairments in processing speed ( 11.7% in FDT- Reading and 10% in FDT- Counting ). The white matter (WM) analyses with DTI * revealed higher axial diffusivity values in post-infected patients compared to controls. * Diffusion tensor imaging tractography , or DTI tractography, is an MRI (magnetic resonance imaging) technique most commonly used to provide imaging of the brain. Our results suggest persistent cognitive impairment and subtle white matter abnormalities in individuals mildly infected , without anxiety or depression symptoms. One intriguing fact is that we observed a high proportion of low average performance in our sample of patients (which has a high average level of education ), including immediate and late verbal episodic memory, phonological and semantic verbal fluency, immediate visuospatial episodic memory, processing speed, and inhibitory control . Although most subjects did not present significant impaired scores compared with the normative data, we speculate that the low average performance affecting different domains may result in a negative impact in everyday life , especially in individuals with high levels of education and cognitive demands .’ ❂ ❦ Note how these findings might negatively affect daily activities that demand sustained cognitive attention and fast reaction times – such as driving a car or motorbike, or piloting a plane. Consider air-traffic control. Consider the impact on healthcare workers whose occupations combine long periods of intense concentration with a need for critical precision. ❂ 📖 (19 Jan 2024 ~ Nature: Scientific Reports) Microstructural brain abnormalities, fatigue, and cognitive dysfunction after mild COVID-19 ➤ © 2024 Nature .
by Harris et al / Current Osteoporosis Reports
•
18 January 2024
‘ Clinical evidence suggests that SARS-CoV-2 may lead to hypocalcemia, altered bone turnover markers, and a high prevalence of vertebral fractures. ’
by Wolfram Ruf / Science
•
18 January 2024
❦ ‘Acute infections with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cause a respiratory illness that can be associated with systemic immune cell activation and inflammation , widespread multi-organ dysfunction , and thrombosis . Not everyone fully recovers from COVID-19, leading to Long Covid, the treatment of which is a major unmet clinical need. Long Covid can affect people of all ages , follows severe as well as mild disease , and involves multiple organs . Patients with Long Covid display signs of immune dysfunction and exhaustion , persistent immune cell activation , and autoimmune antibody production , which are also pathological features of acute COVID-19. The complement system is crucial for innate immune defense by effecting lytic destruction of invading micro-organisms, but when uncontrolled, it causes cell and vascular damage . The complement cascade is activated by antigen–antibody complexes in the classical pathways or in the lectin pathway by multimeric proteins (lectins) that recognize specific carbohydrate structures, which are also found on the SARS-CoV-2 spike protein that facilitates host cell entry. Both pathways may contribute to the pronounced complement activation in acute COVID-19. Long Covid symptoms include a postexertional exhaustion reminiscent of other post-viral illnesses , such as myalgic encephalomyelitis ( ME ) – chronic fatigue syndrome ( MECFS ) with suspected latent viral reactivation . Antibody titer changes in Long Covid patients indicate an association of fatigue with reactivation of latent Epstein-Barr virus ( EBV ) infections , and Cervia-Hasler et al found that the severity of Long Covid symptoms is associated with cytomegalovirus ( CMV ) reactivation . A better understanding of the connections between viral reactivation, persistent interferon signaling, and autoimmune pathologies promises to yield new insights into the thromboinflammation associated with Long Covid. Although therapeutic interventions with coagulation and complement inhibitors in acute COVID-19 produced mixed results, the pathological features specific for Long Covid suggest potential interventions for clinical testing. Microclots are also observed in ME-CFS patients , indicating crucial interactions between complement, vWF, and coagulation-mediated fibrin formation in post-viral syndromes. A better definition of these interactions in preclinical and clinical settings will be crucial for the translation of new therapeutic concepts in chronic thromboinflammatory diseases .’ ❂ 📖 (18 Jan 2024 ~ Science) Immune damage in Long Covid ➤ © 2024 Wolfram Ruf / Science .
by Michael Merschel / American Heart Association
•
16 January 2024
“I would argue that COVID-19 is not a disease of the lungs at all. It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system.”
by Shajahan et al / Frontiers in Aging Neuroscience
•
8 January 2024
‘[COVID-19’s] ability to invade the central nervous system through the hematogenous and neural routes, besides attacking the respiratory system, has the potential to worsen cognitive decline in Alzheimer’s disease patients. The severity of this issue must be highlighted.’
by Appelman et al / Nature Communications
•
4 January 2024
Post-exertional malaise (PEM) is a marked physical or mental fatigue and deterioration of symptoms occurring after physical , cognitive , social or emotional exertion that would have been tolerated previously. Symptoms typically worsen 12 to 48 hours after such activities , and can last for days , weeks or months , making it difficult to manage or predict. PEM is a hallmark symptom of myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS), and is commonly reported by people with Post-COVID-19 Syndrome (PCS/‘Long Covid’). PEM can be mitigated by activity management , or ‘ pacing ’.
by Carolyn Barber / Fortune & Outbreak Updates
•
14 December 2023
❦ ‘Al-Aly’s study undertook a comparative analysis of 94 pre-specified health outcomes and found that over 18 months of follow-up, COVID was associated with a “ significantly increased risk ” for 64 of them, or nearly 70% . The disease’s enhanced risk list includes everything from cardiac arrest , stroke , chronic kidney disease , and cognitive impairment to mental health and fatigue , characteristics often associated with long COVID. By comparison, the seasonal flu was associated with increased risk in only 6 of the 94 conditions specified. Further, while COVID increased the risks for almost all the organ systems studied, the flu heightened risk primarily for the pulmonary ( lung ) system . Those findings, Al-Aly says, suggest that “ COVID is really a multi-systemic disease , and flu is more a respiratory virus ”.’ ❂ 📖 (14 Dec 2023 ~ Fortune) COVID-19 v. Flu: A ‘much more serious threat,’ new study into long-term risks concludes ➤ 📖 (14 Dec 2023 ~ The Lancet) Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study ➤ © 2023 Carolyn Barber / Fortune .
by Bland et al / Occupational Medicine
•
11 December 2023
❦ ‘As a consequence of their occupation, doctors and other healthcare workers were at higher risk of contracting coronavirus disease 2019 (COVID-19), and more likely to experience severe disease compared to the general population. Post-acute COVID (Long COVID) in UK doctors is a substantial burden. Insufficient respiratory protection could have contributed to occupational disease, with COVID-19 being contracted in the workplace , and resultant post-COVID complications. Although it may be too late to address the perceived determinants of inadequate protection for those already suffering with Long COVID, more investment is needed in rehabilitation and support of those afflicted .’ ❂ 📖 (11 Dec 2023 ~ Occupational Medicine) Post-acute COVID-19 complications in UK doctors: results of a cross-sectional survey ➤
by Pearson-Stuttard et al / The Lancet (Regional Health Europe)
•
1 December 2023
❦ 'For middle-aged adults ( 50–64 ) in this period [June 2022 – June 2023 ], the relative excess for almost all causes of death examined was higher than that seen for all ages .' ➲ ‘Since July 2020, the Office for Health Improvement and Disparities (OHID) has published estimates of excess mortality. In the period from week ending 3rd June 2022 to 30th June 2023 , excess deaths for all causes were relatively greatest for 50–64 year olds ( 15% higher than expected ), compared with 11% higher for 25–49 and < 25 year olds , and about 9% higher for over 65 year old groups. Several causes, including cardiovascular diseases , show a relative excess greater than that seen in deaths from all-causes ( 9% ) over the same period (week ending 3rd June 2022–30th June 2023), namely: all cardiovascular diseases ( 12% ), heart failure ( 20% ), ischaemic heart diseases ( 15% ), liver diseases ( 19%) , acute respiratory infections ( 14% ), and diabetes ( 13% ). For middle-aged adults (50–64) in this 13-month period, the relative excess for almost all causes of death examined was higher than that seen for all ages . Deaths involving cardiovascular diseases were 33% higher than expected, while for specific cardiovascular diseases, deaths involving ischaemic heart diseases were 44% higher , cerebrovascular diseases 40% higher and heart failure 39% higher . Deaths involving acute respiratory infections were 43% higher than expected and for diabetes , deaths were 35% higher . Deaths involving liver diseases were 19% higher than expected for those aged 50–64 , the same as for deaths at all ages. Looking at place of death, from 3rd June 2022 to 30th June 2023 there were 22% more deaths in private homes than expected compared with 10% more in hospitals . The greatest numbers of excess deaths in the acute phase of the pandemic were in older adults. The pattern now is one of persisting excess deaths which are most prominent in relative terms in middle-aged and younger adults , with deaths from CVD [cardiovascular] causes and deaths in private homes being most affected.’ ❂ ➲ [C19.Life Note ] : Considering their findings and conclusion, I’m not sure why the authors would choose to use the term ‘post-pandemic’ in this title – when their evidence points to an on-going pandemic, fueled by continuing high rates of infection, that is now simply killing younger age-groups than previously seen.] ❂ 📖 (1 Dec 2023 ~ The Lancet (Regional Health Europe) Excess mortality in England post Covid-19 pandemic: implications for secondary prevention ➤ © 2023 Pearson-Stuttard et al / The Lancet (Regional Health Europe) .
by Outbreak Updates
•
24 November 2023
❦ SARS-CoV-2 infection precipitates a molecular cascade that reactivates latent viral agents. Infection doesn’t just pass through the body’s defenses but rather reprograms them. It reactivates dormant pathogens and perpetuates a cycle of chronic immune activation. Long COVID sufferers are burdened with a significantly higher prevalence of immune responses to certain DNA viruses – namely, Epstein-Barr Virus (EBV)* and Parvovirus B19 – than those in good health. * Epstein-Barr Virus (EBV) is a common human virus that spreads primarily through saliva. It is a member of the herpes virus family and is found all over the world. Most people will get infected with EBV in their lifetime and will not have any symptoms. Elevated levels of antibodies against these viruses in Long COVID patients not only signal potential viral reactivations. It also suggests a reality where SARS-CoV-2 may be inciting a smoldering activation of chronic viral infections. ❂ 📖 (9 Nov 2023 ~ European Heart Journal) Sequential activation of DNA viruses by the RNA virus SARS-CoV-2 in patients with long COVID syndrome ➤ © 2023 Outbreak Updates ➲
by Martin et al / Journal of Neurology
•
7 November 2023
❦ ‘It is now well established that post-COVID syndrome ( PCS ) represents a serious complication in a substantial number of patients following SARS-CoV-2 infection. PCS is diagnosed when COVID-19-related symptoms persist for more than 3 months. It can occur even after an initially mild to moderate course of infection , and comprises a large variety of symptoms . Around 30% of PCS patients show neurological and neuropsychiatric sequelae , such as fatigue , depressive symptoms , and cognitive dysfunction . These are experienced as particularly debilitating, as they have detrimental effects on daily functioning in PCS patients and hamper a successful return to their jobs. Fatigue is a frequent and one of the most debilitating symptoms in post-COVID syndrome (PCS). Recently, we proposed that fatigue is caused by hypoactivity of the brain’s arousal network and reflected by a reduction of cognitive processing speed . Eighty-eight PCS patients with cognitive complaints and 50 matched healthy controls underwent neuropsychological assessment. Seventy-seven patients were subsequently assessed at 6-month follow-up. Patients showed cognitive slowing indicated by longer reaction times compared to control participants in a simple-response tonic alertness task and in all more complex tasks requiring speeded performance . Reduced alertness correlated with higher fatigue . Alertness dysfunction remained unchanged at 6-month follow-up and the same was true for most attention tasks and cognitive domains .’ ❂ 📖 (7 Nov 2023 ~ Journal of Neurology) Persistent cognitive slowing in post-COVID patients: longitudinal study over 6 months ➤ © 2023 Journal of Neurology .
by Rich Haridy / New Atlas
•
31 October 2023
A layperson-level overview from New Atlas on how all variants of SARS-CoV-2 – the virus that causes COVID-19 – are ‘neuroinvasive’ , meaning that all can infect or enter the brain and the nervous system . (From July 2023 Nature Communications study: ‘Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants’.)
by Outbreak Updates
•
11 October 2023
❦ Your brain is a vast city. The roads (myelin) in this city let cars move efficiently. Oligodendrocytes are the construction workers who maintain these roads. As we age, these workers slow down, causing traffic jams and slower thoughts. Enter SARS-CoV-2, the destructive rioter. It doesn’t just disrupt traffic; it damages the roads and chases away the construction crews. Weeks after the riot, the city still struggles to function, with long-lasting road damages and traffic jams. This is the ‘brain fog’ of post-COVID life. ❂ 📖 (24 Sep 2023 ~ Aging and Disease) Role of Microglia, Decreased Neurogenesis and Oligodendrocyte Depletion in Long COVID-Mediated Brain Impairments ➤ © 2023 Outbreak Updates ➲
by Outbreak Updates
•
10 October 2023
❦ Your lungs are balloons made of the finest silk, allowing them to expand and contract effortlessly with each breath. SARS-CoV-2 is as a needle, puncturing and tearing this delicate fabric. In an attempt to heal, the body patches up the punctures, but instead of the original silk, it uses rough patches. These patches – scarring or fibrosis – make parts of the lung rigid, restricting its once flawless expansion. With each subsequent infection, more patches appear, further suffocating the lung’s true function. The virus doesn’t just infect. It sabotages the very essence of our breath. ❂ 📖 (6 Apr 2022 ~ Annals of Medicine and Surgery) Post COVID-19 pulmonary fibrosis; a meta-analysis study ➤ © 2023 Outbreak Updates ➲
by Merck and Co.
•
16 September 2023
❦ ‘The most common causes of acquired lymphocytopenia include: ➲ Protein-energy undernutrition. ➲ HIV infection. ➲ COVID-19 . ➲ Certain other viral infections. Patients with HIV infection routinely have lymphocytopenia, which arises from destruction of CD4+ T cells infected with the HIV virus. Patients with COVID-19 also frequently have lymphocytopenia ( 35% to 83% of patients ) . Lower lymphocyte counts portend a poor prognosis and an increased likelihood of requiring ICU admission and of dying from the disease. The cause of the lymphocytopenia is not completely understood, but COVID-19 can directly infect lymphocytes, and a cytokine-related apoptosis of the cells is likely. ➲ Lymphocytopenia is most often due to AIDS , and recently COVID-19 , or undernutrition, but it also may be inherited or caused by various infections, drugs, or autoimmune disorders. ➲ Patients have recurrent viral , bacterial , fungal , or parasitic infections .’ ❂ 📖 (Accessed 16 Sep 2023 ~ Merck & Co.) Entry for 'Lymphocytopenia' in Merck Manual ➤ © 2023 Merck & Co .
by Sauve et al / eBioMedicine: Lancet Discovery Science
•
12 September 2023
❦ ‘We have recently demonstrated a causal link between loss of gonadotropin-releasing hormone ( GnRH ), the master molecule regulating reproduction , and cognitive deficits during pathological aging , including Down syndrome and Alzheimer’s disease. Olfactory and cognitive alterations , which persist in some COVID-19 patients, and long-term hypotestosteronaemia in SARS-CoV-2-infected men are also reminiscent of the consequences of deficient GnRH, suggesting that GnRH system neuroinvasion could underlie certain post-COVID symptoms and thus lead to accelerated or exacerbated cognitive decline . We explored the hormonal profile of COVID-19 patients and targets of SARS-CoV-2 infection in post-mortem patient brains and human fetal tissue. We found that persistent hypotestosteronaemia in some men could indeed be of hypothalamic origin , favouring post-COVID cognitive or neurological symptoms , and that changes in testosterone levels and body weight over time were inversely correlated. Infection of olfactory sensory neurons and multifunctional hypothalamic glia called tanycytes highlighted at least two viable neuroinvasion routes . Furthermore, GnRH neurons themselves were dying in all patient brains studied , dramatically reducing GnRH expression. Human fetal olfactory and vomeronasal epithelia , from which GnRH neurons arise, and fetal GnRH neurons also appeared susceptible to infection . Putative GnRH neuron and tanycyte dysfunction following SARS-CoV-2 neuroinvasion could be responsible for serious reproductive , metabolic , and mental health consequences in long-COVID and lead to an increased risk of neurodevelopmental and neurodegenerative pathologies over time in all age groups .’ ❂ 📖 (12 Sep 2023 ~ eBioMedicine: Lancet Discovery Science) Long-COVID cognitive impairments and reproductive hormone deficits in men may stem from GnRH neuronal death ➤ © 2023 eBioMedicine: Lancet Discovery Science .
by Antiviral Marketing
•
11 September 2023
❦ — “I don’t know anyone with Long Covid.” — “Everyone I know is tired.” ❂ © 2023 Antiviral Marketing . ➲
by Di Chiara et al / Acta Paediatrica
•
9 September 2023
❦ Children have largely been unaffected by severe COVID-19 compared to adults, but data suggest that they may have experienced new conditions after developing the disease. We compared 1656 exposed and 1656 unexposed children from 1 February 2020 to 30 November 2021. We found significantly higher risks for some new conditions in exposed children, including mental health issues and neurological problems . The overall excess risk for new-onset conditions after COVID-19 was 78% higher in the exposed than unexposed children. ❂ 📖 (9 Sep 2023 ~ Acta Paediatrica) Comparative study showed that children faced a 78% higher risk of new-onset conditions after they had COVID-19 ➤ © 2023 Di Chiara et al / Acta Paediatrica.
by Parotto et al / The Lancet
•
17 July 2023
❦ ‘Individuals with SARS-CoV-2 infection can develop symptoms that persist well beyond the acute phase of COVID-19 or emerge after the acute phase, lasting for weeks or months after the initial acute illness. The post-acute sequelae of COVID-19 (PASC) , which include physical, cognitive, and mental health impairments, are known collectively as long COVID or post-COVID-19 condition (PCC) . The proportion of patients affected by post-COVID-19 condition might be in the range of 10–30% of those infected with SARS-CoV-2, although understanding of this condition is still evolving. Socio-economic factors are fundamental determinants of health after COVID-19. Individuals from low-income and middle-income countries, those from marginalised communities, and those who are socially disadvantaged are probably disproportionately affected. The post-COVID-19 condition is systemic, affecting various organ systems. PCC results in: an increased use of healthcare resources ; a decreased quality of life ; an increased susceptibility to subsequent viral or bacterial infection ; and leads to heightened vulnerability to perioperative morbidity and mortality for individuals who require a surgical procedure for any (unrelated) indication. With a large and growing global population of survivors of COVID-19, the impact on individuals, healthcare systems, communities, and society is likely to be substantial. At present, there are no specific treatments for post-COVID-19-condition.’ ❂ 📖 (17 July 2023 ~ The Lancet) Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations ➤ © 2023 Parotto et al / The Lancet.
by Altmann et al / Nature
•
11 July 2023
❦ ‘Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new healthcare challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with Long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein-Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. The oncoming burden of Long COVID faced by patients, healthcare providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it.’ ❂ 📖 (11 July 2023 ~ Nature Reviews: Immunology) The immunology of long COVID ➤ © 2023 Altmann et al / Nature.
by Dr. Kelly Fearnley, NHS (England)
•
4 July 2023
‘Healthcare workers must be provided with respiratory protection and the air quality in hospitals be monitored and improved through the installation of ventilation systems and air filter units.’ ✾
by NHS Palliative Care Medicine Consultant
•
25 June 2023
❦ “Feeling validated that life is ‘back to normal’ as you see all of those unmasked people around you in restaurants, shops and cinemas? I’ll let you in on a little secret. Those who recognise the risk and who would be masked up aren’t even there. They are busy elsewhere staying healthy. More than 400 million now have Long Covid; a disease from Covid that can impact any organ system, and is proven to cause damage to the brain, heart, lung, kidney, gut, immune and multiple other systems. That’s one in 20 globally. How come you don’t know anyone with it? It’s one of three likely reasons… 1. They have been sick so long that they do what most chronically ill people do when they are asked, “How are you?” They say, “I’m fine”. 2. They don’t recognise the relation of their recent heart attack/memory impairment/new diabetes to their Covid illness in the last year. 3. It’s because they aren’t at that restaurant, movie, theatre, work night out as they don’t fancy worsening their already awful situation with a further infection. Out of sight, out of mind. Even those who know someone with Long Covid will minimise it, as it doesn’t fit with the general narrative that Covid is over. It’s too much cognitive dissonance for most people to handle. Easier to believe that everything’s OK, and it must “just be them being anxious”. It’s not over. I’ll let you in on another special secret; it’s not anxiety. It’s a calm determination to maintain health, in the full knowledge of what Covid can do.” © 2023 NHS Palliative Care Medicine Consultant .
by NHS Medical Consultant
•
25 June 2023
❦ I have seen a disproportionate number of young patients with advanced cancer over the last two years. They used to stand out: now it’s every week. The evidence points to direct Covid-driven mechanisms for rises in cancer risk. Will you hear about it in the news? Of course not. Covid’s over. It’s just anxiety now if you’re thinking about it. Except it’s not. It’ll take years for people to accept this. It’ll be too late. A number of my oncology colleagues have been commenting on how they’ve never seen such aggressively-progressive cancers in all their careers since Covid arrived. I’ve been seeing it as all these patients come to me. It isn’t normal. Alarm bells should be ringing loudly. The evidence: 📖 (22 Mar 2023 ~ Global Journal of Life Sciences and Biological Research) Cancer Related-Genes Enriched in Peripheral Blood Mononuclear Cells (PBMCs) of COVID-19 Patients: A Bioinformatics Study ➤ ‘SARS-CoV-2 can be considered a potential risk factor for increasing the probability of developing cancer.’ Study 1: 📖 (7 Jun 2022 ~ Frontiers in Oncology) SARS-CoV-2 M Protein Facilitates Malignant Transformation of Breast Cancer Cells ➤ ‘Coronavirus disease 2019 (COVID-19) has spread faster due to the emergence of SARS-CoV-2 variants, which carry an increased risk of infecting patients with comorbidities, such as breast cancer.’ Study 2: 📖 (9 Aug 2022 ~ Journal of Infection ) Is SARS-CoV-2 an oncogenic virus? ➤ ‘Gene expression of p53 [tumour suppressor] is downregulated in blood of COVID-19 patients. Downregulation persists at least 24 weeks after infection in long COVID-19 patients. Long-term reduction of p53 could have impact on carcinogenesis.’ 📖 (9 Aug 2022 ~ Journal of Infection) Letter to the editor: Is SARS-CoV-2 an oncogenic virus? ➤ Study 3: 📖 (22 Mar 2023 ~ Global Journal of Life Sciences and Biological Research) Cancer related-genes enriched in peripheral blood mononuclear cells (PBMCs) of COVID-19 patients. A bioinformatics study ➤ ‘Numerous cancer-related genes up-regulated in SARS-CoV-2-infected patients, particularly those genes participating in the cell-cycle regulation or engaged in cellular senescence processes.’ Study 4: 📖 (2 Jun 2023 ~ Biochimie) Possible cancer-causing capacity of COVID-19: Is SARS-CoV-2 an oncogenic agent? ➤ ‘One of the most worrying long-term effects of infection is the potential to induce malignant neoplasms, which will be a major health concern over the coming decades. SARS-CoV-2 infection affects many mechanisms that play a crucial role in cancer onset and progression including cell-cycle regulation, the RAAS system and inflammation / proliferation signaling pathways.’ ❂ Related reading : 📖 (9 Aug 2021 ~ Nature: Scientific Reports) More than 50 Long-term effects of COVID-19: a systematic review and meta-analysis ➤ 📖 (21 Jun 2021 ~ Nature: Scientific Reports) The risk of pancreatic adenocarcinoma following SARS-CoV family infection ➤ 📖 (4 Mar 2021 ~ Nature: Scientific Reports) COVID-19 engages clinical markers for the management of cancer and cancer-relevant regulators of cell proliferation, death, migration, and immune response ➤ 📖 (28 Jan 2021 ~ Nature: Scientific Reports) Meta-analysis of host transcriptional responses to SARS-CoV-2 infection reveals their manifestation in human tumors ➤ 📖 (25 Jan 2010 ~ Nature: Oncogene) Viral epigenome in human tumorigenesis ➤ 📖 (Dec 2006 ~ Yale Journal of Biology and Medicine) Viruses and human cancer ➤ ❂ © 2023 NHS Medical Consultant .
by Martinez-Marmol & Hilliard / Queensland Brain Institute
•
8 June 2023
❦ Researchers at The University of Queensland have discovered viruses such as SARS-CoV-2 can cause brain cells to fuse, initiating malfunctions that lead to chronic neurological symptoms. SARS-CoV-2, the virus that causes COVID-19, has been detected in the brains of people with 'Long COVID' months after their initial infection. "We discovered COVID-19 causes neurons to undergo a cell fusion process, which has not been seen before," Professor Hilliard said. "After neuronal infection with SARS-CoV-2, the spike S protein becomes present in neurons, and once neurons fuse, they don't die." "They either start firing synchronously, or they stop functioning altogether." As an analogy, Professor Hilliard likened the role of neurons to that of wires connecting switches to the lights in a kitchen and a bathroom. "Once fusion takes place, each switch either turns on both the kitchen and bathroom lights at the same time, or neither of them," he said. "It's bad news for the two independent circuits." The discovery offers a potential explanation for persistent neurological effects after a viral infection. "In the current understanding of what happens when a virus enters the brain, there are two outcomes – either cell death or inflammation," Dr Martinez-Marmol said. "But we've shown a third possible outcome, which is neuronal fusion." Dr Martinez-Marmol said numerous viruses cause cell fusion in other tissues, but also infect the nervous system and could be causing the same problem there. "These viruses include HIV, rabies, Japanese encephalitis, measles, herpes simplex virus and Zika virus," he said. “Our research reveals a new mechanism for the neurological events that happen during a viral infection. “This is potentially a major cause of neurological diseases and clinical symptoms that is still unexplored.” ❂ 📖 (7 June 2023 ~ Science Advances) SARS-CoV-2 infection and viral fusogens cause neuronal and glial fusion that compromises neuronal activity ➤ 📖 (8 June 2023 ~ Queensland Brain Institute) COVID-19 can cause brain cells to 'fuse' ➤ © 2023 Martinez-Marmol & Hilliard / Queensland Brain Institute / University of Queensland.
by NHS Palliative Medicine Consultant
•
19 May 2023
❦ “What if Covid has been causing mass cognitive impairment and we are all living in an increasingly stupid society? Mad things could happen with that: imagine if hospitals got rid of masks or people started to believe Covid was just a cold? I know that’s far-fetched, but imagine!” ❂ © 2023 NHS Palliative Medicine Consultant .
by The John Snow Project
•
5 May 2023
❦ Prior to 2020, there were four endemic human coronaviruses – OC43, NL-63, 229E, and HKU1 – which were known to cause 10 to 15 percent of common colds – or the ‘Common Cold Coronaviruses’ (CCCs). From at least the 1970s, we’ve known that infection with these coronaviruses does not lead to lasting protection from reinfection – this is textbook knowledge. CCCs are not just colds – they can cause severe pneumonias, and exhibit a risk profile very similar to SARS-CoV-2 with age. If reinfection really did strengthen immunity against CCCs, then older people would be the least affected – because they would have been regularly infected with diverse variants of these viruses in their past. But that is not the case – and SARS-CoV-2 is not a CCC. SARS-CoV-2 has a wide array of accessory proteins that silence and disrupt our normal immune responses. As we get older, our immune systems start to lose their effectiveness – and we become more susceptible to disease. This process is called immunosenescence . Repeated exposure to a virus like SARS-CoV-2 is fast-tracking more people into immunosenescence at ever-earlier ages, with potentially serious repercussions for their health and longevity. SARS-CoV-2 is a particularly nasty virus that can also trigger the hyperactivation of our own immune systems to cause severe disease. Infection by SARS-CoV-2 has been shown to lead to an increase in autoantibodies and autoimmune disease. Approximately 25 percent of people who develop an autoimmune disease will experience multiple autoimmune syndrome, and will risk a cascade of autoimmune conditions. SARS-CoV-2, like its 2002 predecessor SARS-CoV-1, is both a respiratory and a systemic virus, with an extremely broad cell-type and tissue-tropism covering nearly the whole body. Its ability to infect and do damage to lungs, hearts, kidneys, cardiovascular systems and brains is particularly well-documented. If each subsequent infection results in additional internal organ and immune-system damage, then at some point the damage accumulated – together with the accelerated immune-system aging and normal aging processes – can reasonably be expected to outweigh the protective benefits of immunity developed from previous infections. SARS-CoV-2 reinfects more frequently than influenza or the common cold, infects a wider range of organs, does more damage and seems capable of persisting in a range of organs. So if SARS-CoV-2 behaves like a textbook virus – but does more damage more quickly and more regularly – at what point does the body reach its tipping point? ❂ There are two versions of this article: a 7-minute read in simplified language ; and the full editorial version complete with references, which is an 18-minute-read and aimed towards the medical and scientific communities . ❦ 7-minute primer ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❦ Full 18-minute editorial ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❂ 📖 (5 May 2023 ~ The John Snow Project) SARS-CoV-2 and "Textbook" Immunity ➤ © 2023 The John Snow Project.
by Costanzo et al / International Journal of Molecular Sciences
•
25 April 2023
❦ ‘Some viruses are known to be associated with the onset of specific cancers. These micro-organisms – oncogenic viruses or oncoviruses – can convert normal cells into cancer cells. Seven oncogenic viruses are known to promote tumorigenesis [tumour creation] in humans: Human papillomavirus (HPV) Hepatitis B and C viruses (HBV, HCV) Epstein-Barr virus (EBV) Human T-cell leukemia virus 1 (HTLV-1) Kaposi sarcoma-associated herpesvirus (KSHV) Merkel cell polyomavirus (MCPyV) Recent research indicates that SARS-CoV-2 infection and COVID-19 progression may predispose recovered patients to cancer onset and accelerate cancer development . This hypothesis is based on the growing evidence regarding the ability of SARS-CoV-2 to modulate oncogenic pathways, promoting chronic low-grade inflammation and causing tissue damage.’ ❂ 📖 (25 Apr 2023 ~ International Journal of Molecular Sciences) Deciphering the Relationship between SARS-CoV-2 and Cancer ➤ © 2023 Costanzo et al / International Journal of Molecular Sciences.
by Negm et al / BMC Infectious Diseases
•
23 April 2023
❦ Critically ill COVID-19 patients are highly susceptible to opportunistic fungal infection due to many factors, including virus-induced immune dysregulation , host-related comorbidities, overuse and misuse of antibiotics or corticosteroids, immune modulator drugs, and the emergencies caused by the pandemic. Fungal coinfection is a common complication of critically ill COVID-19 patients admitted to the ICU. Candidiasis , aspergillosis , and mucormycosis are the most common COVID-19-associated fungal infections and have a great impact on mortality rates . ❂ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ © 2023 Negm et al / BMC Infectious Diseases.
by Herrera et al / Nature: Scientific Reports
•
19 April 2023
❦ The results presented here reveal that at least 85% [of the 214 patients with post COVID-19 syndrome] exhibit deficits in one neuropsychological test . Also, the youngest patients were those who showed the most marked and heterogeneous cognitive impairment , while the oldest patients maintained their cognitive functions preserved to a greater extent with only a mild impairment in attention and speed processing. ❂ 📖 (19 Apr 2023 ~ Nature: Scientific Reports) Cognitive impairment in young adults with post COVID-19 syndrome ➤ © 2023 Herrera et al / Nature.
by Sayyadi et al / Annals of Hematology
•
19 April 2023
❦ ‘COVID-19 patients have a hypercoagulability state, and thrombosis is a life-threatening complication of them.’ ✻ Hypercoagulability , also known as thrombophilia , is a condition in which there is an abnormally increased tendency towards blood clotting . ‘From the early days of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) outbreak to the present, clinical and basic studies have indicated that coronavirus disease 2019 (COVID-19) may be associated with coagulopathy ( CAC ), which is involved in its related morbidity and mortality. Deep vein thrombosis ( DVT ) and pulmonary embolism ( PE ) are common in COVID-19 patients and are remarkably high in the intensive care unit (ICU)–admitted patients. CAC can lead to the formation of circulating microthrombi and macrothrombi which can involve multiple sites, including the lungs , brain , heart , and visceral organs like kidneys and spleen . There is a close relationship between the immune system and coagulation. The components of the hemostatic system play a role in the body’s immunity, and the activation of the immune system strongly influences the hemostatic system. Abnormal activation of the immune system may promote the growth of pathologies associated with thrombosis. COVID-19 is accompanied by an immune-cell hyperactivation and excessive production of proinflammatory cytokines , known as “ cytokine storm ”. CAC is theorized to result from dysregulated interactions between the immune and coagulation systems .’ ❂ 📖 (19 Apr 2023 ~ Annals of Hematology) Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement ➤ © 2023 Annals of Hematology .
by Chen et al / Journal of Medical Virology
•
18 April 2023
❦ 'The risk of herpes zoster (HZ) [ shingles ] remained significantly higher [ +60% ] in patients with COVID-19, compared with those without COVID-19. The higher risk of HZ in the COVID-19 cohort compared with that in the non-COVID-19 cohort remained consistent across subgroup analyses regardless of vaccine status, age, or sex. The risk of HZ within a 12-month follow-up period was significantly higher in patients who had recovered from COVID-19 compared with that in the control group.' ❂ 📖 (18 Apr 2023 ~ Journal of Medical Virology) Long-term risk of herpes zoster following COVID-19: A retrospective cohort study of 2 442 686 patients ➤ © 2023 Journal of Medical Virology.
by Wang et al / International Journal of Molecular Sciences
•
18 April 2023
❦ ‘Pulmonary arterial hypertension (PAH) is a pulmonary vascular disease characterized by the progressive elevation of pulmonary arterial pressures.’ Pulmonary Arterial Hypertension ( PAH ) is a progressive lung disease that affects the heart and lungs . It is caused when the tiny arteries in the lungs become thickened and narrowed , causing abnormally high blood pressure in the pulmonary artery . Symptoms include shortness of breath during exercise, fainting spells , dizziness , swelling of the ankles or legs , chest pain , and a racing pulse . ‘It is becoming increasingly apparent that inflammation contributes to the pathogenesis and progression of PAH. Several viruses are known to cause pulmonary arterial hypertension (PAH) , such as SARS-CoV-2 , Human Endogenous Retrovirus K (HERV-K), and Human Immunodeficiency Virus ( HIV ), in part due to acute and chronic inflammation .’ ❂ 📖 (18 Apr 2023 ~ International Journal of Molecular Sciences) Human Endogenous Retrovirus, SARS-CoV-2, and HIV Promote PAH via Inflammation and Growth Stimulation ➤ © 2023 International Journal of Molecular Sciences .
by Sharma & Jagadeesh / Nature Reviews: Rheumatology
•
12 April 2023
❦ The full picture of post-COVID-19 autoimmune diseases and their prevalence is lacking despite numerous case reports and small series. Two studies that use large cohorts now highlight that SARS-CoV-2 infection is linked to a substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases . The reports by Chang et al and Tesch et al provide a comprehensive overview of diverse new-onset autoimmune conditions after COVID-19. In addition, an earlier preprint of a retrospective matched cohort analysis using data from the Clinical Practice Research Datalink Aurum database of 458,147 SARS-CoV-2-infected and 1,818,929 uninfected adults across England between 31 January 2020 and 30 June 2021 reported that the incidence of type 1 diabetes mellitus , inflammatory bowel disease and psoriasis are significantly associated with SARS-CoV-2 infection. Some of the earliest evidence that SARS-CoV-2 infection leads to dysregulated immune responses came from paediatric patients who presented with multisystem inflammatory syndrome in children (MIS-C) , which, as the name indicates, involves diffuse organ system involvement and a clinical spectrum that overlaps with other hyperinflammatory syndromes , such as Kawasaki disease , toxic-shock syndrome , and macrophage activation syndrome . Since the start of the pandemic, many researchers have also reported isolated cases of adults with various post-COVID-19 autoimmune conditions. ❂ 📖 (12 Apr 2023 ~ Nature Reviews: Rheumatology) High risk of autoimmune diseases after COVID-19 ➤ © 2023 Sharma & Jagadeesh / Nature.
by Linseman Laboratory / University of Denver
•
4 April 2023
❦ The Linseman Laboratory is studying the long-term brain health effects of COVID-19 in individuals with and without traumatic brain injury (TBI). Preliminary data suggest that those with a history of both COVID-19 and TBI experience more severe Long COVID symptoms, a higher symptom burden , and more frequent symptoms . Those who reported having COVID-19 and TBI reported worse depressive symptoms , worse functional outcomes , and increased fatigue . ❂ 📖 (4 Apr 2023 ~ SciTechDaily) Researchers Discover Connection Between Traumatic Brain Injury and Long COVID ➤ © 2023 Linesman Laboratory / University of Denver / SciTechDaily.
by Dr. Kevin Kavanagh, MD / Infection Control Today
•
31 March 2023
‘We are entering a phase of long COVID and chronic disability.’ ❂ ❦ ‘As the numbers of hospitalizations and deaths are dropping, many individuals declare the pandemic all but over, comforted by the belief that infections are mild and less dangerous than the seasonal flu. However, the scientific literature these last few weeks has been filled with deeply concerning reports. We are entering a phase of long COVID and chronic disability. The number of COVID-19 cases in the United States is unknown since our case reporting system has become unreliable and substantially undercounts cases. In England, as of the week ending March 7, 2023, 1 in 40 people is positive for COVID-19 , and reinfections are frequently occurring. It is estimated that as of November 9, 2022, 94% of the U.S. population has been infected by SARS-CoV-2 , and 65% of the United States population has been infected multiple times . The odds of self-reported long COVID were 28% less after the second infection. Unfortunately, the damage of long COVID from a second infection adds to the first . One of the most concerning long-term effects of COVID-19 is immune dysfunction or hypofunction . Confirmatory research was reported this week, and summarized in a National Institute of Health news release which stated: ‘… findings suggest that SARS-CoV-2 infection damages the CD8⁺ T cell response , an effect akin to that observed in earlier studies showing long-term damage to the immune system after infection with viruses such as hepatitis C or HIV .’ The authors conclude that this dysfunction causes lasting damage and may ‘contribute to long COVID, perhaps rendering patients unable to respond robustly to subsequent infections by SARS-CoV-2 variants or other pathogens .’ * * 📖 (20 Mar 2023 ~ National Institutes for Health) SARS-CoV-2 infection weakens immune-cell response to vaccination ➤ These findings mirror those reported by Files et al who state: ‘Overall, expression of these activation and exhaustion markers indicated more severe immune dysregulation of CD8 ⁺ T cells in the hospitalized group.’ And they found that ‘ CD8⁺ T cell expression of exhaustion markers increased in non-hospitalized individuals over time ’. * * 📖 (4 Jan 2021 ~ Journal of Clinical Investigation) Sustained cellular immune dysregulation in individuals recovering from SARS-CoV-2 infection ➤ The authors’ finding of damage to the immune system “akin” to HIV is very concerning, as is the amplification of this result in the NIH news release. Infection Control Today previously reported that the probable cause of the surges in infections we are seeing is an immune dysfunction caused by COVID-19 . With minimal public health interventions, Sweden also experienced surges in respiratory syncytial virus (RSV) cases. Most recently, Sweden has undergone a significant surge in seasonal flu, with reports from the Public Health Agency of Sweden of unusually severe cases. These [Swedish influenza] cases have occurred in ‘... people under the age of 18 without underlying disease or condition, and have been very seriously ill with complications such as myocarditis or encephalitis.’ Other diseases are also rising , exemplified by reports of record-high severe Streptococcal infections and Candida auris . These spikes in infections caused by multiple pathogens are associated with the SARS-CoV-2 pandemic and the mounting evidence of post-COVID-19 immune dysfunction. Vaccinations can not only reduce the incidence of severe disease, but can also help to prevent long COVID, reducing the incidence by 30% to 40%. However, we have expressed concern regarding the bivalent booster’s effectiveness, and reported a rapid waning of booster-induced immunity in the elderly. [See Footnote.] Recently, researchers from the United States found that the relative bivalent booster effectiveness at 5 to 7 months in preventing hospitalizations relative to monovalent vaccine dosages (2, 3, or 4) was 42% and 59% compared to no vaccination. Using the third vaccine dose as a baseline, the UK Health Security Agency found that an additional (fourth) vaccine dosage had effectiveness against hospitalizations at 10 weeks of only 50% .’ Source: 📖 (21 Mar 2023 ~ Infection Control Today) COVID-19: Study Suggests Long-term Damage to Immune System ➤ ❂ Footnote: On waning vaccine effectiveness * ‘Vaccine effectiveness is an important point. Although much of the younger population received a get-out-of-hospital free card for the latest variant, senior citizens were in its crosshairs. During the last 6 months (since May of 2022), those over the age of 75 had a higher rate of hospitalizations than in the Delta surge; those between the ages of 65 and 75 had approximately the same. Both age groups continue to be at high risk for death and disability. However, data showed that for those 65 years of age and older, the monovalent vaccine’s (2 or more doses) effectiveness for preventing hospitalizations fell to 28% in less than a year. Results were worse for those individuals under 65 years – only 19%.’ * 📖 (24 Feb 2023 ~ Infection Control Today) How Soon Is Another Booster Needed? Durability of Vaccine-Induced Immunity ➤ ❂ © 2023 Infection Control Today . ➲