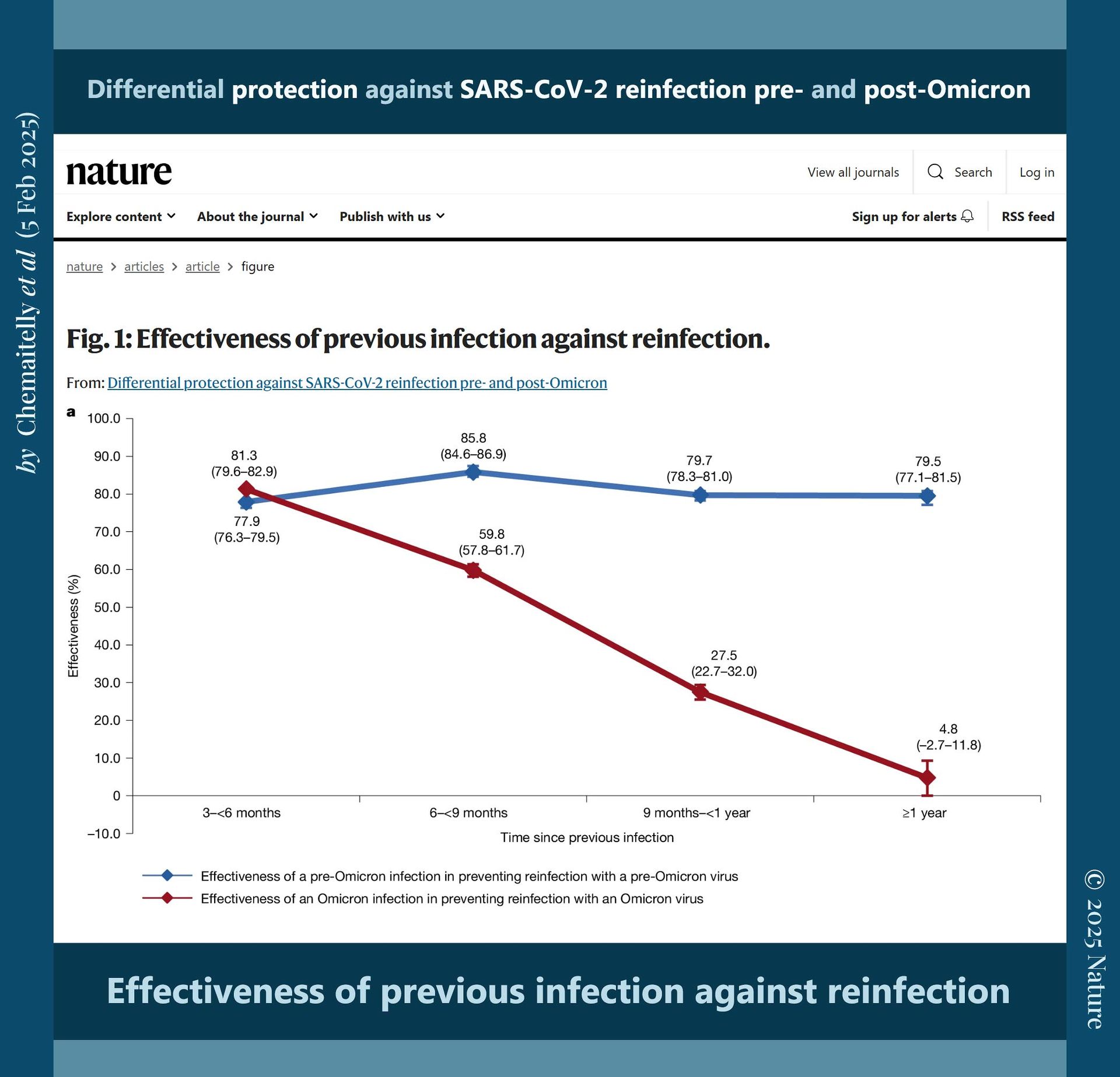
‘The arrival of the Omicron variant marked a major shift, introducing numerous extra mutations in the spike gene compared with earlier variants.
Before Omicron, natural infection provided strong and durable protection against reinfection, with minimal waning over time.
However, during the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year.’
‘Effectiveness of previous infection against reinfection
(Omicron).’
➤
📖
(5 Feb 2025 ~ Nature)
‘Differential protection against SARS-CoV-2 reinfection pre- and post-Omicron’.
© 2025
Chemaitelly
et al
/
Nature.
❦ The
‘Omicron’ Era
(late 2021–).
➲
Data accessed:
7 September 2025.
➲
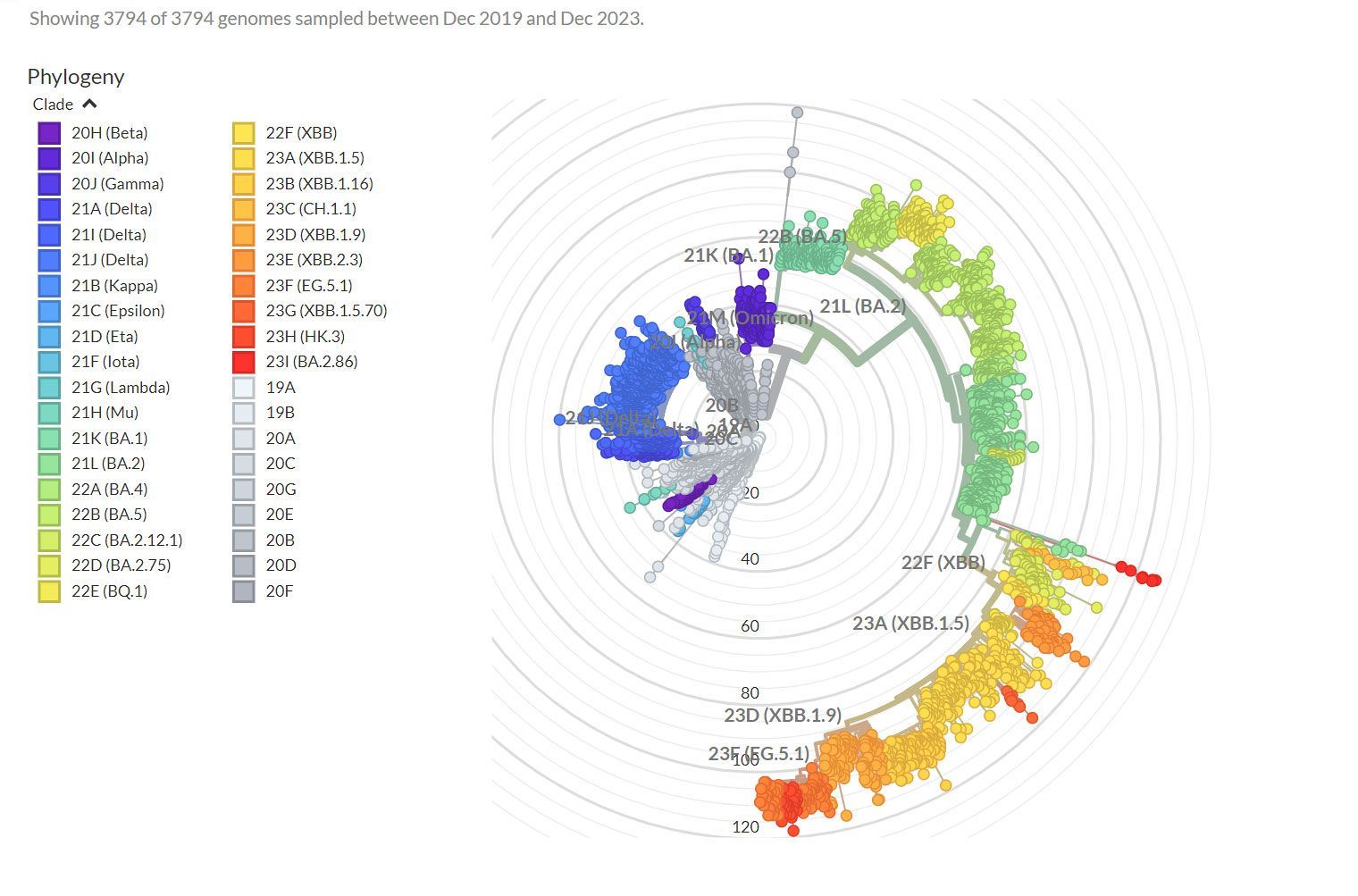
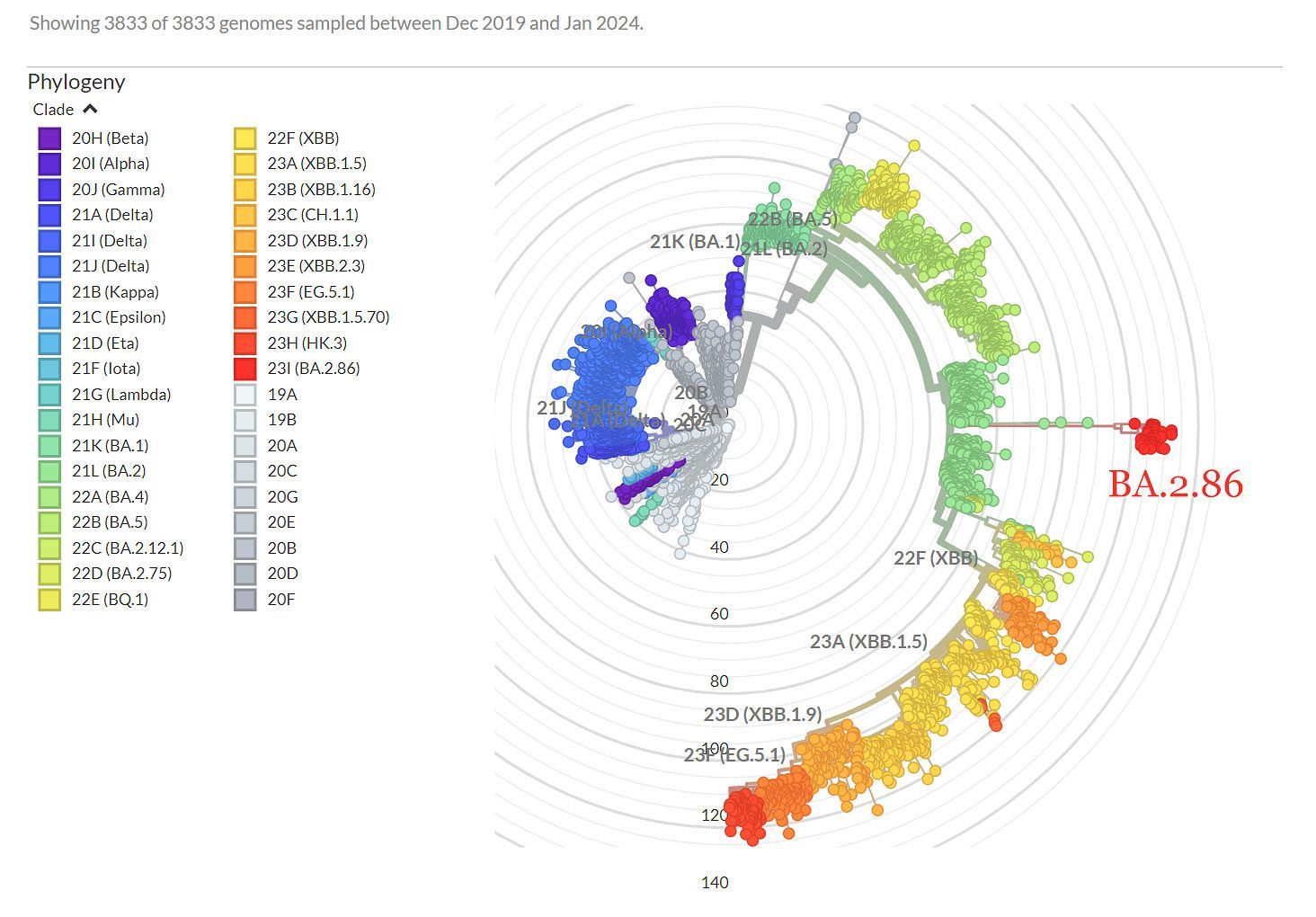
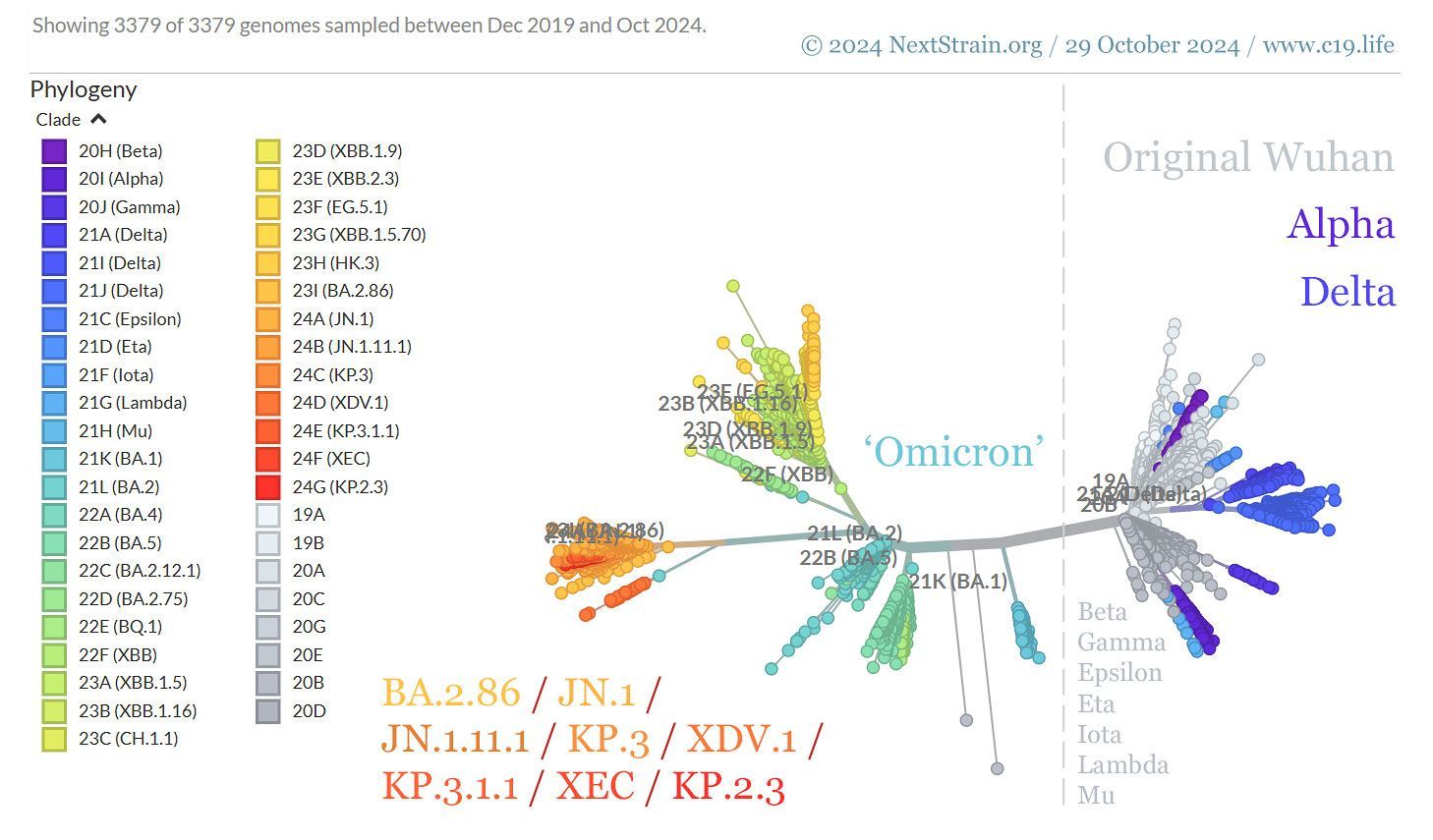
Genomic epidemiology of SARS-CoV-2 since pandemic start, by date.
© 2025
NextStrain.org
/ GISAID.org.
❦
On SARS-CoV-2 reinfections, and their cumulative danger
📖
(5 Feb 2025 ~ Nature)
Differential protection against SARS-CoV-2 reinfection pre- and post-Omicron ➤
‘The arrival of the
Omicron variant
marked a
major shift, introducing numerous extra mutations in the spike gene compared with earlier variants.
Before Omicron,
natural infection provided
strong
and
durable protection
against
reinfection, with
minimal waning
over time.
However, during the
Omicron era,
protection was
robust only
for those
recently infected,
declining rapidly over time
and
diminishing
within
a year.’
© 2025
Chemaitelly
et al
/
Nature.
“Anything that is more transmissible will kill in two ways.
Infecting more people.
Worsening pressure on healthcare.”
Dr. Noor Bari, Emergency Medicine
(2023)
➲
📖
(20 Mar 2025 ~ Canadian Broadcasting Corporation)
Beyond long COVID – how reinfections could be causing silent long-term organ damage ➲
“There was a recent
2024 study
showing us that individuals who
survive an
acute COVID-19 infection – these are not individuals who are getting diagnosed with long COVID – on average
will lose somewhere in the neighbourhood of
two to six IQ points
per infection.”
© 2025
David Putrino /
Radio-Canada ~ Canadian Broadcasting Corporation (CBC).
📖
(27 Mar 2024 ~ BMC Infectious Diseases)
The symptoms and interval of Omicron SARS-CoV-2 reinfection among healthcare workers in a hospital of Southern China: a cross-sectional study ➤
‘The main symptoms during the first infection in this Omicron wave were fever and sore throat, while sore throat was the main symptom in the reinfection; the
average interval
for
SARS-CoV-2
[COVID-19]
reinfection
was
149.91 days.
The
reasons for COVID-19
reinfection are
multifaceted, primarily including
low antibody levels, the
shortened duration
of
immune protection
provided by antibodies, the
mutation
of
viral strains,
non-adherence
to
epidemic prevention measures
by the population,
hesitancy
towards
vaccination, and
public fatigue
due to the prolonged pandemic.’
© 2024
Ma
et al
/
BMC Infectious Diseases.
📖
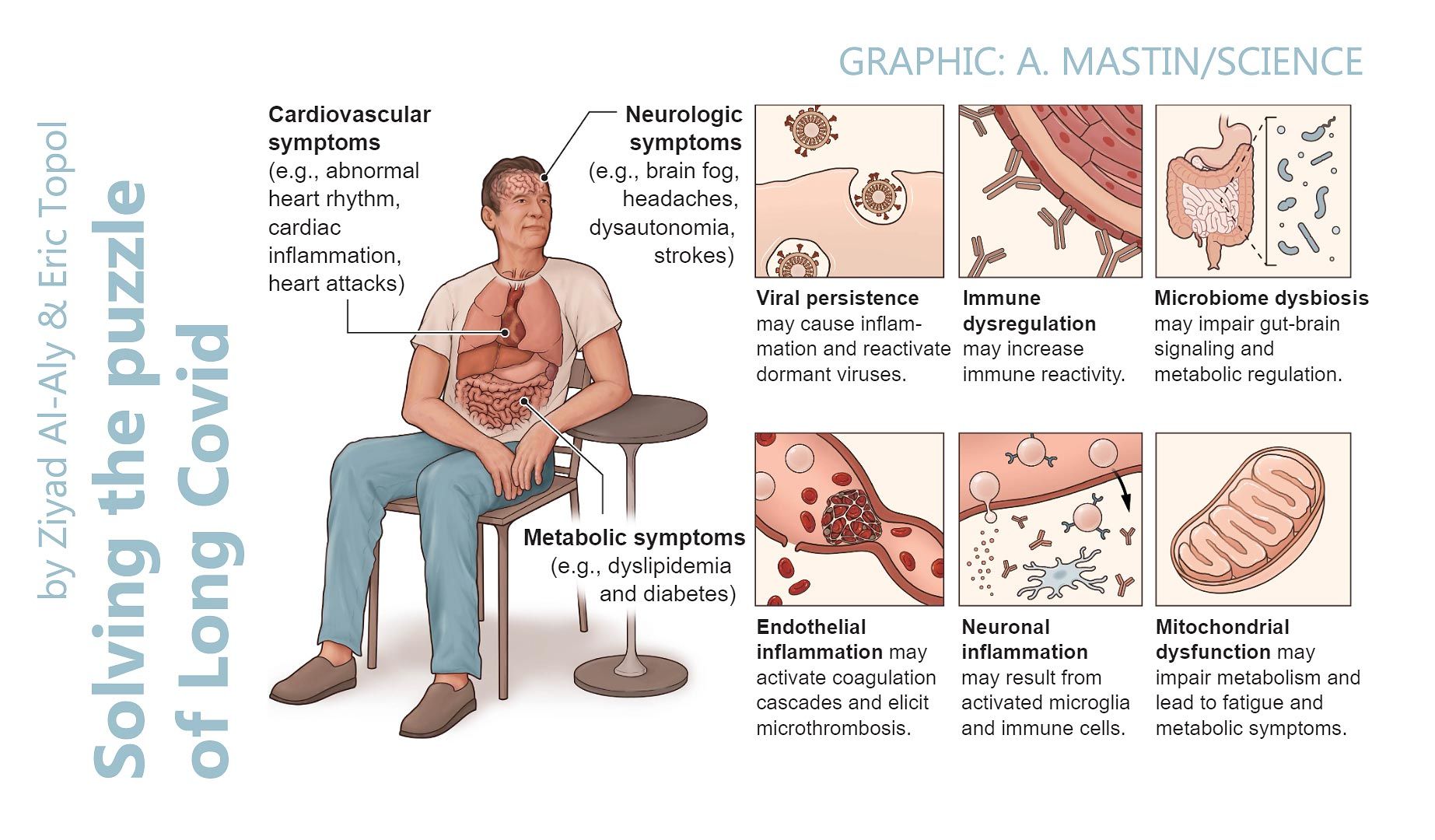
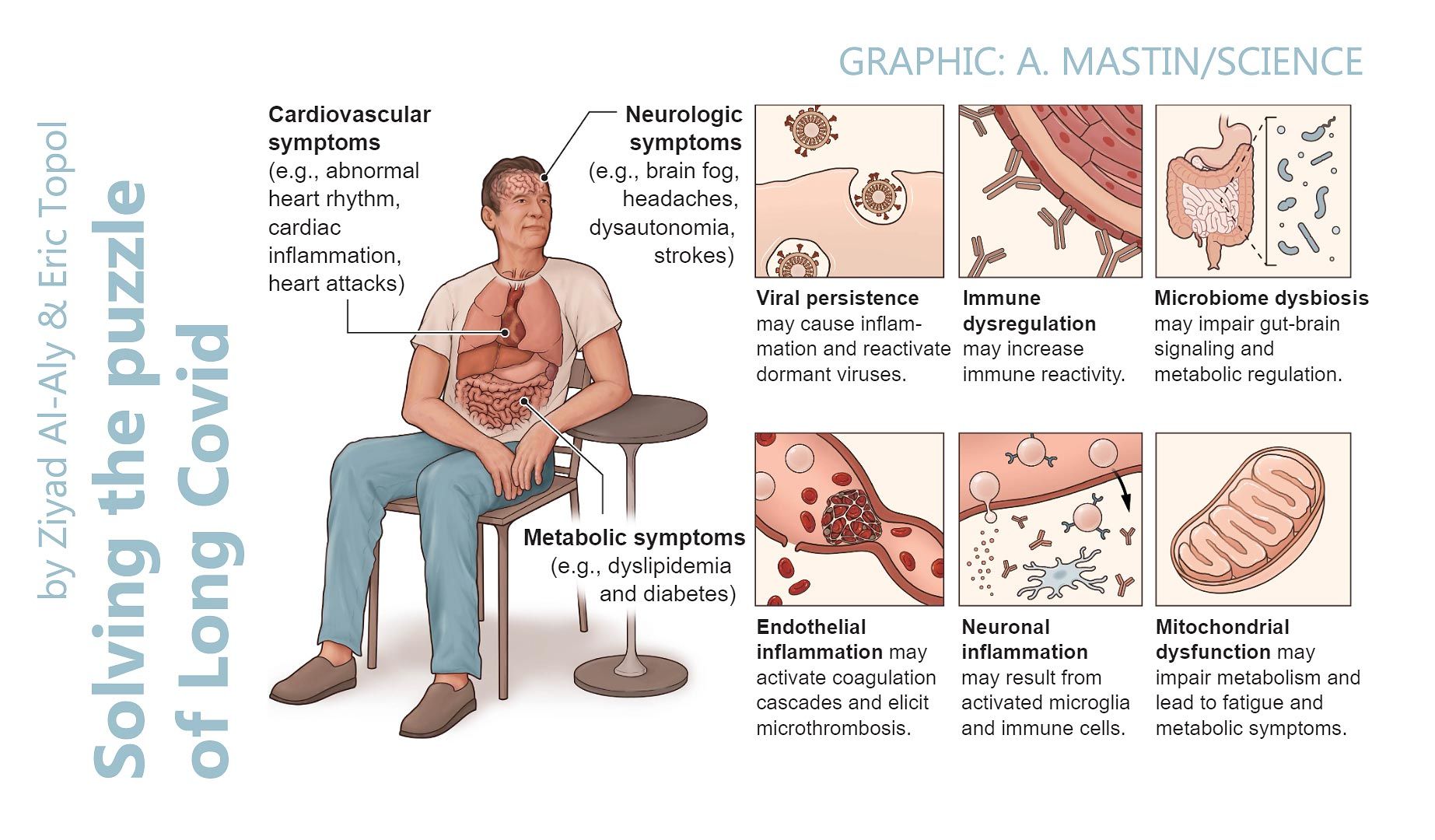
(22 Feb 2024 ~ Science)
Solving the puzzle of Long Covid ➲
‘Reinfection, which is now the
dominant type of
SARS-CoV-2
infection, is not inconsequential; it can
trigger de novo Long Covid
[PASC] or
exacerbate its
severity.
Each reinfection contributes additional risk of Long Covid:
cumulatively, two infections yield a higher risk of Long Covid than one infection, and three infections yield a higher risk than two infections.’
© 2024
Al-Aly & Topol
/
Science.
📖
(2 Feb 2024 ~ Nature: Communications)
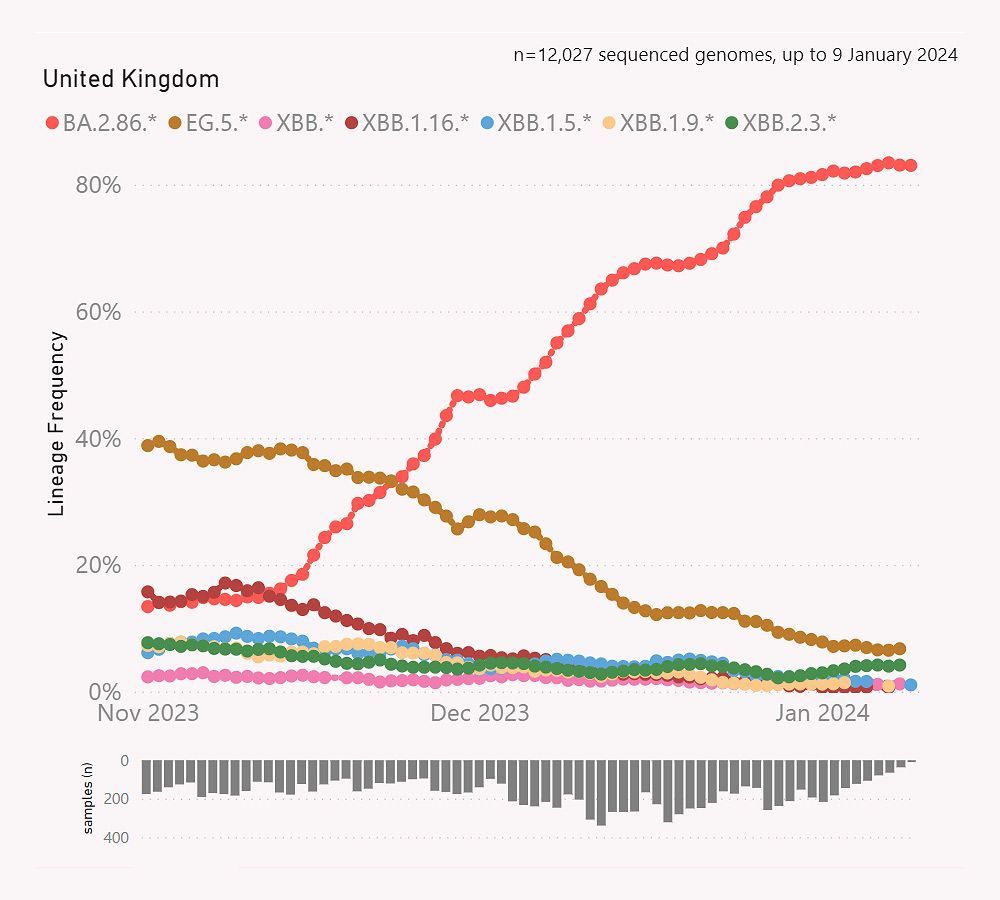
Risk of SARS-CoV-2 reinfection during multiple Omicron variant waves in the UK general population ➤
‘The
estimated risk
of confirmed
reinfection
in the
Omicron waves
is
high, and is associated with both
viral evolution
and
waning immunity, but confirmed reinfections have
lower viral loads
and
fewer symptoms
than the first identified infections.
Additional protection
from
vaccination
also
decreases over time.
Given the
waning immunity
from
previous
infection
and
vaccination, and the
stronger immune evasion
from
most recent Omicron variants,
reinfection risk remains high, and on-going evaluation of hybrid immunity against emerging dominant variants remains important to
pandemic control
and
vaccination policy.
Further public health measures
may be
needed
to help
protect vulnerable people
from
reinfection.’
© 2024
Wei
et al
/
Nature: Communications.
📖
(25 May 2022 ~ Nature: Medicine)
Long COVID after breakthrough SARS-CoV-2 infection ➤
‘At 6 months after infection, beyond the first 30 days of illness, compared to contemporary controls, people with
breakthrough SARS-CoV-2 infection (‘BTI’, or
reinfection) exhibited a
higher risk of
death and
incident post-acute sequelae, including
cardiovascular,
coagulation and
hematologic,
gastrointestinal,
kidney,
mental health,
metabolic,
musculoskeletal and
neurologic
disorders.’
© 2022
Al-Aly, Bowe & Xie / Nature.
“If you are letting yourself get infected and taking no precautions against passing it on, you are not a passive bystander for your next infection.
You’ve participated in creating it.”
Dr. Noor Bari, Emergency Medicine
(2024)
➲
❦
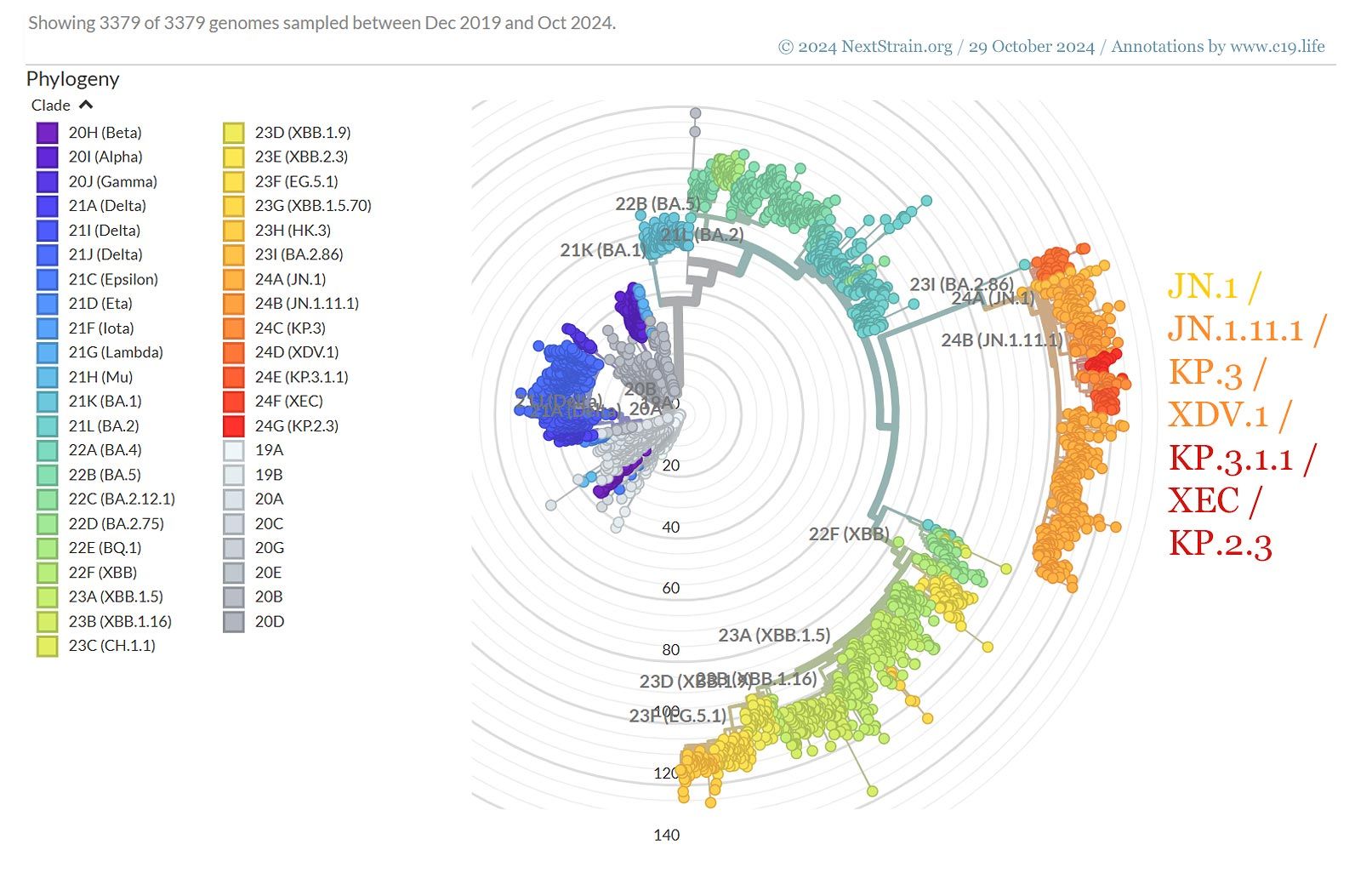
SARS-CoV-2 (COVID-19)
variants of concern
(VOC), and ‘Omicron’.
➲
Data accessed:
29 October 2024.
➲
Genomic epidemiology of SARS-CoV-2 since pandemic start.
➲
© 2024
NextStrain.org
/ GISAID.org.
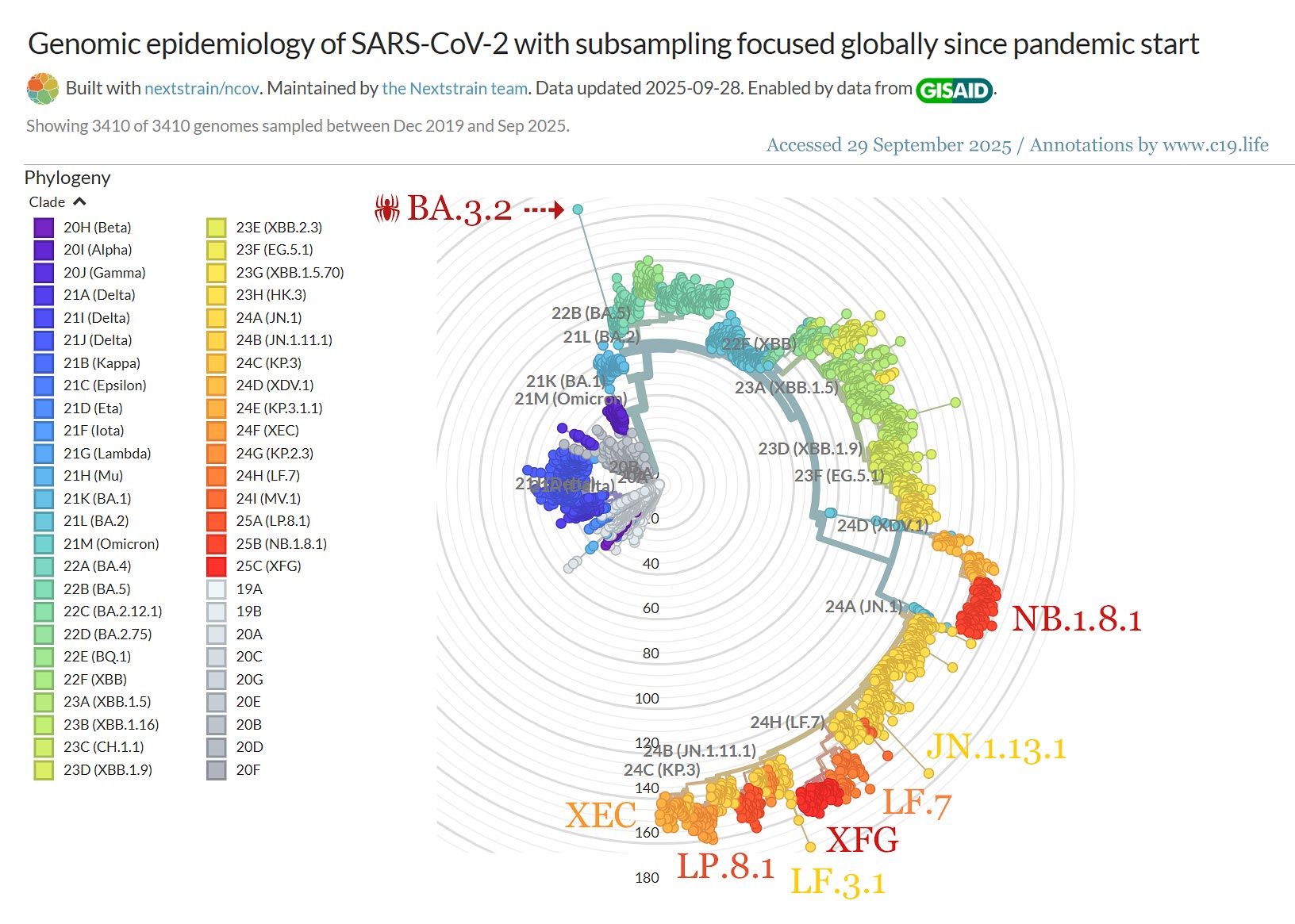
❦
SARS-CoV-2 (COVID-19)
variants of concern
(VOC), and ‘Omicron’.
➲
Data accessed:
29 September 2025.
➲
Genomic epidemiology of SARS-CoV-2 since pandemic start.
➲
© 2025
NextStrain.org
/
GISAID.org.
by C19.Life... et al
•
7 September 2025
‘Vaccine effectiveness against SARS-CoV-2 [COVID-19] infection declines markedly with time and Omicron variants.’ from ‘Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection and severe outcomes in adults’ by Zhou et al / European Respiratory Review (2024).
by David Putrino ❂ Sonya Buyting ~ Radio-Canada / Canadian Broadcasting Corporation
•
20 March 2025
CBC Radio-Canada interview with long COVID [PASC] researcher David Putrino from the Icahn School of Medicine at Mount Sinai in New York.
by Chemaitelly et al / Nature
•
5 February 2025
‘Before Omicron, natural infection provided strong and durable protection against reinfection, with minimal waning over time. However, during the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year.’
by Al-Aly & Topol / Science
•
22 February 2024
‘Reinfection, which is now the dominant type of SARS-CoV-2 infection, is not inconsequential; it can trigger de novo Long Covid or exacerbate its severity. Each reinfection contributes additional risk of Long Covid: cumulatively, two infections yield a higher risk of Long Covid than one infection, and three infections yield a higher risk than two infections.’
by Meng et al / The Lancet: eClinical Medicine
•
17 February 2024
❦ ‘The occurrences of respiratory disorders among patients who survived for 30 days after the COVID-19 diagnosis continued to rise consistently, including asthma , bronchiectasis , COPD , ILD , PVD * , and lung cancer . * COPD = Chronic obstructive pulmonary disease . ILD = Interstitial lung disease . PVD = Peripheral vascular disease . With the severity of the acute phase of COVID-19, the risk of all respiratory diseases increases progressively. Besides, during the 24-months follow-up, we observed an increasing trend in the risks of asthma and bronchiectasis over time, which indicates that long-term monitoring and meticulous follow-up of these patients is essential. These findings contribute to a more complete understanding of the impact of COVID-19 on the respiratory system and highlight the importance of prevention and early intervention of these respiratory sequelae of COVID-19. In this study, several key findings have been further identified. Firstly, our research demonstrates a significant association between COVID-19 and an increased long-term risk of developing various respiratory diseases. Secondly, we found that the risk of respiratory disease increases with severity in patients with COVID-19, indicating that it is necessary to pay attention to respiratory COVID-19 sequelae in patients, especially those hospitalized during the acute stage of infection. This is consistent with the findings of Lam et al., who found that the risk of some respiratory diseases (including chronic pulmonary disease, acute respiratory distress syndrome and ILD) increased with the severity of COVID-19. Notably, however, our study found that asthma and COPD remained evident even in the non-hospitalized population. This emphasizes that even in cases of mild COVID-19, the healthcare system should remain vigilant. Thirdly, we investigated differences in risk across time periods, as well as the long-term effects of COVID-19 on respiratory disease. During the 2-years follow-up period, the risks of COPD, ILD, PVD and lung cancer decreased, while risks of asthma and bronchiectasis increased. Fourthly, our study showed a significant increase of the long-term risk of developing asthma, COPD, ILD, and lung cancer diseases among individuals who suffered SARS-CoV-2 reinfection. This finding emphasizes the importance of preventing reinfection of COVID-19 in order to protect public health and reduce the potential burden of SARS-CoV-2 reinfection. Interestingly, vaccination appears to have a potentially worsening effect on asthma morbidity compared with other outcomes. This observation aligns with some previous studies that have suggested a possible induction of asthma onset or exacerbation by COVID-19 vaccination. It suggests that more care may be necessary for patients with asthma on taking the COVID vaccines. The underlying mechanisms associated with COVID and respiratory outcomes are not fully understood, but several hypotheses have been proposed. First, SARS-CoV-2 can persist in tissues (including the respiratory tract), as well as the circulating system for an extended period of time after the initial infection. This prolonged presence of the virus could directly contribute to long-term damage of the respiratory tissues, consequently leading to the development of various respiratory diseases. Second, it has been observed that SARS-CoV-2 infection can lead to prolonged immunological dysfunctions, including highly activated innate immune cells, a deficiency in naive T and B cells, and increased expression of interferons and other pro-inflammatory cytokines. These immune system abnormalities are closely associated with common chronic respiratory diseases – asthma, bronchiectasis, COPD, as well as the development of lung cancer. Next, SARS-CoV-2 itself has been shown to drive cross-reactive antibody responses, and a range of autoantibodies were found in patients with COVID-19. In conclusion, our research adds to the existing knowledge regarding the effects of COVID-19 on the respiratory system. Specifically, it shows that the risk of respiratory illness increases with the severity of infection and reinfection. Our findings emphasize the importance of providing extended care and attention to patients previously infected with SARS-CoV-2.’ ❂ 📖 (17 Feb 2024 ~ The Lancet: eClinical Medicine) Long-term risks of respiratory diseases in patients infected with SARS-CoV-2: a longitudinal, population-based cohort study ➤ © 2024 The Lancet: eClinical Medicine .
by Dr. Lisa Iannattone, Assistant Professor of Dermatology
•
7 July 2023
❦ “The truth is that SARS2 is so contagious, so virulent, and reinfects so easily that there is no off-ramp for masking in healthcare. At least not without better vaccines and therapeutics that actually stop transmission and prevent Long Covid, Cardiovascular Covid and Neurocovid.”
by The John Snow Project
•
5 May 2023
❦ Prior to 2020, there were four endemic human coronaviruses – OC43, NL-63, 229E, and HKU1 – which were known to cause 10 to 15 percent of common colds – or the ‘Common Cold Coronaviruses’ (CCCs). From at least the 1970s, we’ve known that infection with these coronaviruses does not lead to lasting protection from reinfection – this is textbook knowledge. CCCs are not just colds – they can cause severe pneumonias, and exhibit a risk profile very similar to SARS-CoV-2 with age. If reinfection really did strengthen immunity against CCCs, then older people would be the least affected – because they would have been regularly infected with diverse variants of these viruses in their past. But that is not the case – and SARS-CoV-2 is not a CCC. SARS-CoV-2 has a wide array of accessory proteins that silence and disrupt our normal immune responses. As we get older, our immune systems start to lose their effectiveness – and we become more susceptible to disease. This process is called immunosenescence . Repeated exposure to a virus like SARS-CoV-2 is fast-tracking more people into immunosenescence at ever-earlier ages, with potentially serious repercussions for their health and longevity. SARS-CoV-2 is a particularly nasty virus that can also trigger the hyperactivation of our own immune systems to cause severe disease. Infection by SARS-CoV-2 has been shown to lead to an increase in autoantibodies and autoimmune disease. Approximately 25 percent of people who develop an autoimmune disease will experience multiple autoimmune syndrome, and will risk a cascade of autoimmune conditions. SARS-CoV-2, like its 2002 predecessor SARS-CoV-1, is both a respiratory and a systemic virus, with an extremely broad cell-type and tissue-tropism covering nearly the whole body. Its ability to infect and do damage to lungs, hearts, kidneys, cardiovascular systems and brains is particularly well-documented. If each subsequent infection results in additional internal organ and immune-system damage, then at some point the damage accumulated – together with the accelerated immune-system aging and normal aging processes – can reasonably be expected to outweigh the protective benefits of immunity developed from previous infections. SARS-CoV-2 reinfects more frequently than influenza or the common cold, infects a wider range of organs, does more damage and seems capable of persisting in a range of organs. So if SARS-CoV-2 behaves like a textbook virus – but does more damage more quickly and more regularly – at what point does the body reach its tipping point? ❂ There are two versions of this article: a 7-minute read in simplified language ; and the full editorial version complete with references, which is an 18-minute-read and aimed towards the medical and scientific communities . ❦ 7-minute primer ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❦ Full 18-minute editorial ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❂ 📖 (5 May 2023 ~ The John Snow Project) SARS-CoV-2 and "Textbook" Immunity ➤ © 2023 The John Snow Project.
More... On variants, immunity, and vaccines
by C19.Life
•
1 November 2025
“We’re going to need a bigger Greek alphabet.”
by C19.Life... et al
•
7 September 2025
‘Vaccine effectiveness against SARS-CoV-2 [COVID-19] infection declines markedly with time and Omicron variants.’ from ‘Effectiveness of COVID-19 vaccines against SARS-CoV-2 infection and severe outcomes in adults’ by Zhou et al / European Respiratory Review (2024).
by Guo et al / The Lancet ~ Infectious Diseases
•
5 June 2025
‘Importantly, NB.1.8.1 shows a balanced profile of ACE2 binding and immune evasion, supporting its potential for future prevalence.’
by Zhang et al / The Lancet ~ Microbe
•
3 June 2025
‘Since late 2024, a potential third major evolutionary shift in SARS-CoV-2 evolution might be unfolding. In November 2024 and January 2025, a highly mutated descendant of the Omicron subvariant BA.3 was detected in South Africa.’
by CIDRAP ❂ Cai et al / The Lancet: Infectious Diseases
•
2 April 2025
‘These findings have important implications for understanding the potential impact of COVID-19 on long-term immune function and susceptibility to pathogens.’
by David Putrino ❂ Sonya Buyting ~ Radio-Canada / Canadian Broadcasting Corporation
•
20 March 2025
CBC Radio-Canada interview with long COVID [PASC] researcher David Putrino from the Icahn School of Medicine at Mount Sinai in New York.
by Chemaitelly et al / Nature
•
5 February 2025
‘Before Omicron, natural infection provided strong and durable protection against reinfection, with minimal waning over time. However, during the Omicron era, protection was robust only for those recently infected, declining rapidly over time and diminishing within a year.’
by Al-Aly & Topol / Science
•
22 February 2024
‘Reinfection, which is now the dominant type of SARS-CoV-2 infection, is not inconsequential; it can trigger de novo Long Covid or exacerbate its severity. Each reinfection contributes additional risk of Long Covid: cumulatively, two infections yield a higher risk of Long Covid than one infection, and three infections yield a higher risk than two infections.’
by Meng et al / The Lancet: eClinical Medicine
•
17 February 2024
❦ ‘The occurrences of respiratory disorders among patients who survived for 30 days after the COVID-19 diagnosis continued to rise consistently, including asthma , bronchiectasis , COPD , ILD , PVD * , and lung cancer . * COPD = Chronic obstructive pulmonary disease . ILD = Interstitial lung disease . PVD = Peripheral vascular disease . With the severity of the acute phase of COVID-19, the risk of all respiratory diseases increases progressively. Besides, during the 24-months follow-up, we observed an increasing trend in the risks of asthma and bronchiectasis over time, which indicates that long-term monitoring and meticulous follow-up of these patients is essential. These findings contribute to a more complete understanding of the impact of COVID-19 on the respiratory system and highlight the importance of prevention and early intervention of these respiratory sequelae of COVID-19. In this study, several key findings have been further identified. Firstly, our research demonstrates a significant association between COVID-19 and an increased long-term risk of developing various respiratory diseases. Secondly, we found that the risk of respiratory disease increases with severity in patients with COVID-19, indicating that it is necessary to pay attention to respiratory COVID-19 sequelae in patients, especially those hospitalized during the acute stage of infection. This is consistent with the findings of Lam et al., who found that the risk of some respiratory diseases (including chronic pulmonary disease, acute respiratory distress syndrome and ILD) increased with the severity of COVID-19. Notably, however, our study found that asthma and COPD remained evident even in the non-hospitalized population. This emphasizes that even in cases of mild COVID-19, the healthcare system should remain vigilant. Thirdly, we investigated differences in risk across time periods, as well as the long-term effects of COVID-19 on respiratory disease. During the 2-years follow-up period, the risks of COPD, ILD, PVD and lung cancer decreased, while risks of asthma and bronchiectasis increased. Fourthly, our study showed a significant increase of the long-term risk of developing asthma, COPD, ILD, and lung cancer diseases among individuals who suffered SARS-CoV-2 reinfection. This finding emphasizes the importance of preventing reinfection of COVID-19 in order to protect public health and reduce the potential burden of SARS-CoV-2 reinfection. Interestingly, vaccination appears to have a potentially worsening effect on asthma morbidity compared with other outcomes. This observation aligns with some previous studies that have suggested a possible induction of asthma onset or exacerbation by COVID-19 vaccination. It suggests that more care may be necessary for patients with asthma on taking the COVID vaccines. The underlying mechanisms associated with COVID and respiratory outcomes are not fully understood, but several hypotheses have been proposed. First, SARS-CoV-2 can persist in tissues (including the respiratory tract), as well as the circulating system for an extended period of time after the initial infection. This prolonged presence of the virus could directly contribute to long-term damage of the respiratory tissues, consequently leading to the development of various respiratory diseases. Second, it has been observed that SARS-CoV-2 infection can lead to prolonged immunological dysfunctions, including highly activated innate immune cells, a deficiency in naive T and B cells, and increased expression of interferons and other pro-inflammatory cytokines. These immune system abnormalities are closely associated with common chronic respiratory diseases – asthma, bronchiectasis, COPD, as well as the development of lung cancer. Next, SARS-CoV-2 itself has been shown to drive cross-reactive antibody responses, and a range of autoantibodies were found in patients with COVID-19. In conclusion, our research adds to the existing knowledge regarding the effects of COVID-19 on the respiratory system. Specifically, it shows that the risk of respiratory illness increases with the severity of infection and reinfection. Our findings emphasize the importance of providing extended care and attention to patients previously infected with SARS-CoV-2.’ ❂ 📖 (17 Feb 2024 ~ The Lancet: eClinical Medicine) Long-term risks of respiratory diseases in patients infected with SARS-CoV-2: a longitudinal, population-based cohort study ➤ © 2024 The Lancet: eClinical Medicine .
by NextStrain.org / GISAID.org
•
21 January 2024
❦ Genomic epidemiology of SARS-CoV-2 with subsampling focused globally since pandemic start. All data and data visualisation by © 2025 NextStrain.org / GISAID.org .
by Mike Honey
•
19 January 2024
❦ Mike Honey’s Variant Visualiser (COVID-19 Genomic Sequence Analysis). The region of ‘Oceania/Australia’ is set by default, as the visualiser was created by Mike Honey , a Data Visualisation and Data Integration specialist in Melbourne, Australia. ➲ Choose your country by clicking on the ‘ Continent, Country, Location ’ dropdown menu in the top-right-hand corner . The variant visualiser is free to use, and is automatically updated every time you open the link. ❂ © 2024 Mike Honey .
by Michael Merschel / American Heart Association
•
16 January 2024
“I would argue that COVID-19 is not a disease of the lungs at all. It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system.”
by Professor Phil Banfield (BMA) & Dr. Barry Jones (CAPA)
•
22 December 2023
‘It is accepted that COVID-19 can be and is spread by the airborne route. The recent evidence given at the UK COVID-19 Inquiry clearly shows that aerosol transmission is a significant, and almost certainly the dominant, route of transmission for COVID-19.’ The British Medical Association (22 Dec 2023)
by Royal College of Nursing (RCN) (UK)
•
21 December 2023
‘The RCN is urging healthcare employers to assess the risk posed by COVID-19 and put appropriate safeguards in place for patients and staff. WHO [has] advised healthcare workers and health facilities to implement universal masking in health facilities, as well as appropriate masking, respirators and other personal protective equipment for health workers caring for suspected and confirmed COVID-19 patients; and to improve ventilation in health facilities.’ ✾ ❦ We’ve contacted chief nursing officers in all four UK countries and the UKHSA to find out what action will be taken in response to WHO’s statement on a new COVID-19 variant of interest. The RCN is asking for a revision to current guidelines , to introduce universal implementation of the two measures advised by the World Health Organization (WHO) to help protect healthcare staff against COVID-19. Earlier this week, in light of the new COVID JN.1 variant, WHO advised healthcare workers and health facilities to: implement universal masking in health facilities , as well as appropriate masking , respirators and other personal protective equipmen t for health workers caring for suspected and confirmed COVID-19 patients ; improve ventilation in health facilities . The existing national infection prevention and control manuals don’t require standardised masking for COVID-19, and decisions on respiratory protective equipment are left to local risk assessments. This is now inconsistent with WHO’s latest advice . We also have concerns about the adequacy of ventilation in general ward and outpatient areas within hospital buildings and believe that action must be taken to assess and improve this. Although evidence suggests that the global public health risks from the new variant are low, WHO has warned that onset of winter could increase the burden of respiratory infections in the Northern hemisphere. This comes when there are already unsustainable pressures on the health service. Figures show that there has been a rise in COVID-19 cases and hospitalisations , and the RCN argues that without proper protections , ill health could continue to rise in nursing staff and impact their ability to deliver safe and effective patient care . WHO has advised that it is continuously monitoring the evidence and will update the JN.1 risk evaluation as needed. The RCN is urging healthcare employers to assess the risk posed by COVID-19 and put appropriate safeguards in place for patients and staff . Our COVID-19 workplace risk assessment toolkit aims to help assess and manage the risks associated with respiratory infections such as COVID-19, highlights the duties of nursing staff in specific roles (such as health and safety reps), has advice for employers and leaders, and provides the latest information on risk assessment. ❂ 📖 (21 Dec 2023 ~ Royal College of Nursing / RCN Magazine) COVID JN.1 variant: RCN seeks assurance on new PPE advice ➤ © 2023 Royal College of Nursing (RCN).
by The World Health Organization (WHO)
•
19 December 2023
❦ ‘Due to its rapidly increasing spread , WHO is classifying the variant JN.1 as a separate variant of interest ( VOI ) from the parent lineage BA.2.86 . It was previously classified as VOI as part of BA.2.86 sublineages. Based on the available evidence, the additional global public health risk posed by JN.1 is currently evaluated as low. Despite this, with the onset of winter in the Northern Hemisphere, JN.1 could increase the burden of respiratory infections in many countries. ➲ Read the risk evaluation: ‘Tracking SARS-CoV-2 variants’ . WHO is continuously monitoring the evidence and will update the JN.1 risk evaluation as needed. Current vaccines continue to protect against severe disease and death from JN.1 and other circulating variants of SARS-CoV-2, the virus that causes COVID-19. COVID-19 is not the only respiratory disease circulating. Influenza, RSV and common childhood pneumonia are on the rise. ➲ WHO advises people to take measures to prevent infections and severe disease using all available tools . These include: • Wear a mask when in crowded, enclosed, or poorly ventilated areas, and keep a safe distance from others, as feasible. • Improve ventilation . • Practise respiratory etiquette – covering coughs and sneezes. • Clean your hands regularly. • Stay up-to-date with vaccinations against COVID-19 and influenza, especially if you are at high risk for severe disease. • Stay home if you are sick . • Get tested if you have symptoms, or if you might have been exposed to someone with COVID-19 or influenza. ✻ ➲ For health workers and health facilities , WHO advises : • Universal masking in health facilities , as well as appropriate masking , respirators and other PPE for health workers caring for suspected and confirmed COVID-19 patients . • Improve ventilation in health facilities. Note : Updated 19 Dec 2023 with additional information for health workers and facilities. ’ ❂ 📖 (19 Jan 2023 ~ WHO / World Health Organization) World Health Organization (WHO) Media Advisory for the COVID-19 variant of interest (VOI) JN.1 ➤ © 2023 WHO / World Health Organization. ❦ Date accessed : 11 Jan 2024 .
by Conor Browne
•
28 November 2023
❦ “If you’re puzzled as to why governments and public health departments almost never mention even the possibility of SARS-CoV-2-induced immune dysregulation, it’s because to do so would be to admit the greatest mistake made in the history of modern health policy.” ❂ © 2023 Conor Browne ➲
by Cat in the Hat
•
22 November 2023
❦ Chris Whitty, from the Covid Inquiry: “The one situation... that you would ever aim to achieve herd immunity is by vaccination . That is the only situation that is a rational policy response.” And yet... the UK is no longer offering vaccines to the vast majority of its working-age population. According to the JCVI member Dr Adam Finn, the UK’s strategy going forward is that: “... most under 65’s will now end up boosting their immunity not through vaccination, but through catching Covid many times .” ➲ (24 Sep 2023 ~ BBC) What you need to know about Covid as new variant rises ➤ Let me translate: The stated aim is to get infected over and over and over again... to protect against being infected over and over and over again! How does this make any sense at all? The government has decided that it is not good “value for money” to actually give the boosters out – even for the age groups who have already had Covid vaccine doses purchased for them (for example, the 50-65 year olds) – so millions of doses [8.5 million] are now destined to be binned, rather than being used. ➲ ‘COVID VACCINE: COST EFFECTIVENESS ASSESSMENT. For the first time ever, the UK government has used a ‘bespoke, non-standard cost-effectiveness assessment’ to decide who would be eligible for the Covid booster this Autumn. In this thread, I explore how this assessment was undertaken…’ ➤ Meanwhile, in many other countries, the booster is open to anyone who wants it . No strict eligibility criteria. Just step forward and get protected. Let’s take a look at a few: 1. THE USA : Covid booster available to EVERYONE aged 6 months and older. The CDC (USA’s Centers for Disease Control ) recommends that everyone ages 6 months and upwards get the updated COVID-19 booster to protect against serious illness. The new vaccine targets the most common circulating variants, and should be available later this week. The full details are here ➤ . 2. CANADA : Covid booster available to EVERYONE aged 6 months and older. Full details are here ➤ . 3. FRANCE : Covid booster available to EVERYONE. Full details are here ➤ . 4. BELGIUM : Covid booster available to EVERYONE. Full details are here ➤ . 5. JAPAN : Covid booster available to EVERYONE aged 6 months and older. Full details are here ➤ . Why is the UK falling so far out of step with so many other countries on their Covid vaccine strategy? How can they justify binning millions of purchased vaccine doses when there are many people who would gladly take them? ➲ ‘So what’s going to happen to the millions of purchased doses which now won’t be used? Well, here’s the real kicker... it seems they’re destined for the bin. A number of alternative uses have been considered, but the conclusion is: “THESE DOSES HAVE NO FEASIBLE ALTERNATIVE USE”. ’ ➤ If the UK government won’t fund deployment of the Covid jab to EVERYONE (as so many other countries do), then why isn’t there at least an option to buy it privately? This model already exists with the flu jab – why is there not the same option for Covid? © 2023 Cat in the Hat ➲
by Rich Haridy / New Atlas
•
31 October 2023
A layperson-level overview from New Atlas on how all variants of SARS-CoV-2 – the virus that causes COVID-19 – are ‘neuroinvasive’ , meaning that all can infect or enter the brain and the nervous system . (From July 2023 Nature Communications study: ‘Neuroinvasion and anosmia are independent phenomena upon infection with SARS-CoV-2 and its variants’.)
by Dr. Adam Finn, Professor of Paediatrics, University of Bristol / Jim Reed, BBC
•
24 September 2023
❦ ‘The emergence of [new SARS-CoV-2 Variant of Interest] BA.2.86 meant a decision was made to bring forward the autumn Covid booster to better protect the most vulnerable this winter. But the new jabs are only available to people over 65 years old – it was the over-50s last year – and those with certain health conditions. That is a tactical decision , says Dr. Adam Finn, Professor of Paediatrics at the University of Bristol. He explained: “When younger people who’ve already had infections and vaccines get Covid [again], they get a cold and a cough and might be off work for a few days. There’s no real value in investing a lot of time and effort immunising them again when there are so many other things for the Health Service to be doing.” [ ❦ Note : Can a 62-year-old be defined as a ‘ younger person ’? Yes, at a pinch, if Mr. Finn compares them to a 78-year-old. What age-group do these ‘ younger people ’ belong to who don’t need vaccinating, and who instead need to be continually reinfected with a highly pathogenic Biohazard-Level 3 virus? Could it be a 32-year-old man or woman hoping to have a baby ? Or the 0 to 19-year-olds , who are the academic professor’s strong suit? ] ‘The reality is then that most under-65s will now end up boosting their immunity not through vaccination , but through catching Covid many times . In general, Prof Finn says each new infection should feel milder with the length of time you are sick reduced [sic] . “Each time you catch it, your immunity gets stronger and broader ,” he adds. ’ ❂ [ Note : This is simply not true, and is staggeringly dangerous. ] ❂ 📖 (24 Sep 2023 ~ Jim Reed, Health Reporter / BBC online) What you need to know about Covid as new variant [BA.2.86] rises ➤ © 2023 BBC .
by Merck and Co.
•
16 September 2023
❦ ‘The most common causes of acquired lymphocytopenia include: ➲ Protein-energy undernutrition. ➲ HIV infection. ➲ COVID-19 . ➲ Certain other viral infections. Patients with HIV infection routinely have lymphocytopenia, which arises from destruction of CD4+ T cells infected with the HIV virus. Patients with COVID-19 also frequently have lymphocytopenia ( 35% to 83% of patients ) . Lower lymphocyte counts portend a poor prognosis and an increased likelihood of requiring ICU admission and of dying from the disease. The cause of the lymphocytopenia is not completely understood, but COVID-19 can directly infect lymphocytes, and a cytokine-related apoptosis of the cells is likely. ➲ Lymphocytopenia is most often due to AIDS , and recently COVID-19 , or undernutrition, but it also may be inherited or caused by various infections, drugs, or autoimmune disorders. ➲ Patients have recurrent viral , bacterial , fungal , or parasitic infections .’ ❂ 📖 (Accessed 16 Sep 2023 ~ Merck & Co.) Entry for 'Lymphocytopenia' in Merck Manual ➤ © 2023 Merck & Co .
by Dr. Noor Bari, Emergency Medicine
•
27 August 2023
❦ “If y’all are busy weakening your immune systems with one virus, let me assure you that there are packs of other pathogens out there waiting to chew on the leftovers.”
by Altmann et al / Nature
•
11 July 2023
❦ ‘Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe. The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new healthcare challenge. Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways. The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia. A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with Long COVID. Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities. Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters. There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein-Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation. The oncoming burden of Long COVID faced by patients, healthcare providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it.’ ❂ 📖 (11 July 2023 ~ Nature Reviews: Immunology) The immunology of long COVID ➤ © 2023 Altmann et al / Nature.
by Conor Browne
•
18 May 2023
❦ “Since January 2020, a substantial part of what I do has, quite simply, been trying to tell the future. That is fundamentally what forecasting is. I have been right far, far more times than I have been wrong. Much as my reputation hangs on accuracy of prediction, I would much rather have been wrong. This is the difference, I think, between people like myself and people who seek to minimise: they want to be right – I want to be wrong. These thoughts often crystallise for me when I write, rather than discuss. Today, I was writing a report for a client and, completely unbidden, a fragment of a quotation from Michael Shaara’s Pulitzer Prize-winning novel ‘The Killer Angels’ came to my mind. I reached for the book on my bookshelf to read it; indulge me while I share it with you: ‘The vision was brutally clear: he had to wonder at the clarity of it. Few things in a soldier’s life were so clear as this, so black-line etched that he could actually see the blue troops for one long bloody moment, going up the long slope to the stony top as if it were already done and a memory already, an odd, set, stony quality to it, as if tomorrow had occurred and there was nothing you could do about it, the way you sometimes feel before a foolish attack, knowing it will fail but you cannot stop it or even run away but must even take part and help it fail.’ I’m telling you all now – and, believe me, I want to be wrong – that if we don’t slow transmission of this virus and develop new treatments and second-generation vaccines, the damage we are allowing to occur to the health of our global population – not just the elderly, the disabled and the vulnerable, but everyone – well, that damage is unsustainable. And the vast majority of that population don’t understand the risk, because they haven’t been given the information. An odd, set, stony quality to it.” © 2023 Conor Browne . ➲
by Conor Browne
•
8 May 2023
❦ ‘A significant part of my professional role is forecasting: that is to say, quantifying the risks faced by commercial and other organisations in the future as a result of SARS-CoV-2 and other pathogens (especially H5N1). As such, I often produce bespoke scenarios for clients – 6 months, 12 months, 24 months into the future – assigning probabilities to each scenario occurring. As this article * makes clear, the risk of the emergence of a new Variant of Concern (VOC) within the next two years is about 20 percent. * 📖 (5 May 2023 ~ CNN) Covid-19 experts say they warned White House about chance of an Omicron-level event within the next two years ➤ Any risk manager reading this will know that this is a highly significant risk. Biological risks do not exist in isolation; rather, they are nested within both the domestic politics of any given jurisdiction, and within geopolitics in general. This is a very important point to remember. The recent declaration by the WHO * has (rightfully) angered many people – but, frankly, it has made little practical difference to what I do professionally. * 📖 (5 May 2023 ~ CNN) WHO says Covid-19 is no longer a global health emergency ➤ The vast majority of national governments essentially stopped addressing C-19 in any serious manner quite some time ago. This is the key domestic political risk that intersects with the biological risk of the emergence of a new VOC. National apathy regarding C-19, combined with the growing mainstreaming of both anti-vax sentiment and a reduction in infection control measures in general (such as dropping respirator use in healthcare environments), has created a very dangerous situation. In short, as a global society, we are less prepared now for either the emergence of another disease with pandemic potential (specifically H5N1 avian influenza), or the emergence of a SARS-CoV-2 VOC that exhibits significant immune evasion around current vaccines, than we were in 2019. If either – or both – of these were to occur within the next couple of years, we would be in deep, deep trouble. Currently, we are allowing SARS-CoV-2 to transmit entirely unchecked; this means that pressures on healthcare systems globally will inexorably continue to increase. Concurrently, the population of many jurisdictions worldwide are now primed to reject even the lightest of societal non-pharmaceutical interventions (NPIs) [ such as respirator/mask mandates ] . This combination virtually guarantees that should an immune-evasive VOC emerge we would see healthcare system collapse in many jurisdictions. The short-term goals of domestic politics (maintaining or attaining political power) relies on shying away from the discussion of anything to do with the pandemic. This is the tragic ground truth that has a high chance of coming back to bite us all very badly soon.’ © 2023 Conor Browne . ➲
by The John Snow Project
•
5 May 2023
❦ Prior to 2020, there were four endemic human coronaviruses – OC43, NL-63, 229E, and HKU1 – which were known to cause 10 to 15 percent of common colds – or the ‘Common Cold Coronaviruses’ (CCCs). From at least the 1970s, we’ve known that infection with these coronaviruses does not lead to lasting protection from reinfection – this is textbook knowledge. CCCs are not just colds – they can cause severe pneumonias, and exhibit a risk profile very similar to SARS-CoV-2 with age. If reinfection really did strengthen immunity against CCCs, then older people would be the least affected – because they would have been regularly infected with diverse variants of these viruses in their past. But that is not the case – and SARS-CoV-2 is not a CCC. SARS-CoV-2 has a wide array of accessory proteins that silence and disrupt our normal immune responses. As we get older, our immune systems start to lose their effectiveness – and we become more susceptible to disease. This process is called immunosenescence . Repeated exposure to a virus like SARS-CoV-2 is fast-tracking more people into immunosenescence at ever-earlier ages, with potentially serious repercussions for their health and longevity. SARS-CoV-2 is a particularly nasty virus that can also trigger the hyperactivation of our own immune systems to cause severe disease. Infection by SARS-CoV-2 has been shown to lead to an increase in autoantibodies and autoimmune disease. Approximately 25 percent of people who develop an autoimmune disease will experience multiple autoimmune syndrome, and will risk a cascade of autoimmune conditions. SARS-CoV-2, like its 2002 predecessor SARS-CoV-1, is both a respiratory and a systemic virus, with an extremely broad cell-type and tissue-tropism covering nearly the whole body. Its ability to infect and do damage to lungs, hearts, kidneys, cardiovascular systems and brains is particularly well-documented. If each subsequent infection results in additional internal organ and immune-system damage, then at some point the damage accumulated – together with the accelerated immune-system aging and normal aging processes – can reasonably be expected to outweigh the protective benefits of immunity developed from previous infections. SARS-CoV-2 reinfects more frequently than influenza or the common cold, infects a wider range of organs, does more damage and seems capable of persisting in a range of organs. So if SARS-CoV-2 behaves like a textbook virus – but does more damage more quickly and more regularly – at what point does the body reach its tipping point? ❂ There are two versions of this article: a 7-minute read in simplified language ; and the full editorial version complete with references, which is an 18-minute-read and aimed towards the medical and scientific communities . ❦ 7-minute primer ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❦ Full 18-minute editorial ~ ‘SARS-CoV-2 and “Textbook” Immunity’ ➤ ❂ 📖 (5 May 2023 ~ The John Snow Project) SARS-CoV-2 and "Textbook" Immunity ➤ © 2023 The John Snow Project.
by Negm et al / BMC Infectious Diseases
•
23 April 2023
❦ Critically ill COVID-19 patients are highly susceptible to opportunistic fungal infection due to many factors, including virus-induced immune dysregulation , host-related comorbidities, overuse and misuse of antibiotics or corticosteroids, immune modulator drugs, and the emergencies caused by the pandemic. Fungal coinfection is a common complication of critically ill COVID-19 patients admitted to the ICU. Candidiasis , aspergillosis , and mucormycosis are the most common COVID-19-associated fungal infections and have a great impact on mortality rates . ❂ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ © 2023 Negm et al / BMC Infectious Diseases.
by Sayyadi et al / Annals of Hematology
•
19 April 2023
❦ ‘COVID-19 patients have a hypercoagulability state, and thrombosis is a life-threatening complication of them.’ ✻ Hypercoagulability , also known as thrombophilia , is a condition in which there is an abnormally increased tendency towards blood clotting . ‘From the early days of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) outbreak to the present, clinical and basic studies have indicated that coronavirus disease 2019 (COVID-19) may be associated with coagulopathy ( CAC ), which is involved in its related morbidity and mortality. Deep vein thrombosis ( DVT ) and pulmonary embolism ( PE ) are common in COVID-19 patients and are remarkably high in the intensive care unit (ICU)–admitted patients. CAC can lead to the formation of circulating microthrombi and macrothrombi which can involve multiple sites, including the lungs , brain , heart , and visceral organs like kidneys and spleen . There is a close relationship between the immune system and coagulation. The components of the hemostatic system play a role in the body’s immunity, and the activation of the immune system strongly influences the hemostatic system. Abnormal activation of the immune system may promote the growth of pathologies associated with thrombosis. COVID-19 is accompanied by an immune-cell hyperactivation and excessive production of proinflammatory cytokines , known as “ cytokine storm ”. CAC is theorized to result from dysregulated interactions between the immune and coagulation systems .’ ❂ 📖 (19 Apr 2023 ~ Annals of Hematology) Status of major hemostatic components in the setting of COVID-19: the effect on endothelium, platelets, coagulation factors, fibrinolytic system, and complement ➤ © 2023 Annals of Hematology .
by Chen et al / Journal of Medical Virology
•
18 April 2023
❦ 'The risk of herpes zoster (HZ) [ shingles ] remained significantly higher [ +60% ] in patients with COVID-19, compared with those without COVID-19. The higher risk of HZ in the COVID-19 cohort compared with that in the non-COVID-19 cohort remained consistent across subgroup analyses regardless of vaccine status, age, or sex. The risk of HZ within a 12-month follow-up period was significantly higher in patients who had recovered from COVID-19 compared with that in the control group.' ❂ 📖 (18 Apr 2023 ~ Journal of Medical Virology) Long-term risk of herpes zoster following COVID-19: A retrospective cohort study of 2 442 686 patients ➤ © 2023 Journal of Medical Virology.
by Sharma & Jagadeesh / Nature Reviews: Rheumatology
•
12 April 2023
❦ The full picture of post-COVID-19 autoimmune diseases and their prevalence is lacking despite numerous case reports and small series. Two studies that use large cohorts now highlight that SARS-CoV-2 infection is linked to a substantially increased risk of developing a diverse spectrum of new-onset autoimmune diseases . The reports by Chang et al and Tesch et al provide a comprehensive overview of diverse new-onset autoimmune conditions after COVID-19. In addition, an earlier preprint of a retrospective matched cohort analysis using data from the Clinical Practice Research Datalink Aurum database of 458,147 SARS-CoV-2-infected and 1,818,929 uninfected adults across England between 31 January 2020 and 30 June 2021 reported that the incidence of type 1 diabetes mellitus , inflammatory bowel disease and psoriasis are significantly associated with SARS-CoV-2 infection. Some of the earliest evidence that SARS-CoV-2 infection leads to dysregulated immune responses came from paediatric patients who presented with multisystem inflammatory syndrome in children (MIS-C) , which, as the name indicates, involves diffuse organ system involvement and a clinical spectrum that overlaps with other hyperinflammatory syndromes , such as Kawasaki disease , toxic-shock syndrome , and macrophage activation syndrome . Since the start of the pandemic, many researchers have also reported isolated cases of adults with various post-COVID-19 autoimmune conditions. ❂ 📖 (12 Apr 2023 ~ Nature Reviews: Rheumatology) High risk of autoimmune diseases after COVID-19 ➤ © 2023 Sharma & Jagadeesh / Nature.
by Dr. Kevin Kavanagh, MD / Infection Control Today
•
31 March 2023
‘We are entering a phase of long COVID and chronic disability.’ ❂ ❦ ‘As the numbers of hospitalizations and deaths are dropping, many individuals declare the pandemic all but over, comforted by the belief that infections are mild and less dangerous than the seasonal flu. However, the scientific literature these last few weeks has been filled with deeply concerning reports. We are entering a phase of long COVID and chronic disability. The number of COVID-19 cases in the United States is unknown since our case reporting system has become unreliable and substantially undercounts cases. In England, as of the week ending March 7, 2023, 1 in 40 people is positive for COVID-19 , and reinfections are frequently occurring. It is estimated that as of November 9, 2022, 94% of the U.S. population has been infected by SARS-CoV-2 , and 65% of the United States population has been infected multiple times . The odds of self-reported long COVID were 28% less after the second infection. Unfortunately, the damage of long COVID from a second infection adds to the first . One of the most concerning long-term effects of COVID-19 is immune dysfunction or hypofunction . Confirmatory research was reported this week, and summarized in a National Institute of Health news release which stated: ‘… findings suggest that SARS-CoV-2 infection damages the CD8⁺ T cell response , an effect akin to that observed in earlier studies showing long-term damage to the immune system after infection with viruses such as hepatitis C or HIV .’ The authors conclude that this dysfunction causes lasting damage and may ‘contribute to long COVID, perhaps rendering patients unable to respond robustly to subsequent infections by SARS-CoV-2 variants or other pathogens .’ * * 📖 (20 Mar 2023 ~ National Institutes for Health) SARS-CoV-2 infection weakens immune-cell response to vaccination ➤ These findings mirror those reported by Files et al who state: ‘Overall, expression of these activation and exhaustion markers indicated more severe immune dysregulation of CD8 ⁺ T cells in the hospitalized group.’ And they found that ‘ CD8⁺ T cell expression of exhaustion markers increased in non-hospitalized individuals over time ’. * * 📖 (4 Jan 2021 ~ Journal of Clinical Investigation) Sustained cellular immune dysregulation in individuals recovering from SARS-CoV-2 infection ➤ The authors’ finding of damage to the immune system “akin” to HIV is very concerning, as is the amplification of this result in the NIH news release. Infection Control Today previously reported that the probable cause of the surges in infections we are seeing is an immune dysfunction caused by COVID-19 . With minimal public health interventions, Sweden also experienced surges in respiratory syncytial virus (RSV) cases. Most recently, Sweden has undergone a significant surge in seasonal flu, with reports from the Public Health Agency of Sweden of unusually severe cases. These [Swedish influenza] cases have occurred in ‘... people under the age of 18 without underlying disease or condition, and have been very seriously ill with complications such as myocarditis or encephalitis.’ Other diseases are also rising , exemplified by reports of record-high severe Streptococcal infections and Candida auris . These spikes in infections caused by multiple pathogens are associated with the SARS-CoV-2 pandemic and the mounting evidence of post-COVID-19 immune dysfunction. Vaccinations can not only reduce the incidence of severe disease, but can also help to prevent long COVID, reducing the incidence by 30% to 40%. However, we have expressed concern regarding the bivalent booster’s effectiveness, and reported a rapid waning of booster-induced immunity in the elderly. [See Footnote.] Recently, researchers from the United States found that the relative bivalent booster effectiveness at 5 to 7 months in preventing hospitalizations relative to monovalent vaccine dosages (2, 3, or 4) was 42% and 59% compared to no vaccination. Using the third vaccine dose as a baseline, the UK Health Security Agency found that an additional (fourth) vaccine dosage had effectiveness against hospitalizations at 10 weeks of only 50% .’ Source: 📖 (21 Mar 2023 ~ Infection Control Today) COVID-19: Study Suggests Long-term Damage to Immune System ➤ ❂ Footnote: On waning vaccine effectiveness * ‘Vaccine effectiveness is an important point. Although much of the younger population received a get-out-of-hospital free card for the latest variant, senior citizens were in its crosshairs. During the last 6 months (since May of 2022), those over the age of 75 had a higher rate of hospitalizations than in the Delta surge; those between the ages of 65 and 75 had approximately the same. Both age groups continue to be at high risk for death and disability. However, data showed that for those 65 years of age and older, the monovalent vaccine’s (2 or more doses) effectiveness for preventing hospitalizations fell to 28% in less than a year. Results were worse for those individuals under 65 years – only 19%.’ * 📖 (24 Feb 2023 ~ Infection Control Today) How Soon Is Another Booster Needed? Durability of Vaccine-Induced Immunity ➤ ❂ © 2023 Infection Control Today . ➲
by Dr. Noor Bari, Emergency Medicine
•
20 February 2023
❦ “I’m vaguely following the chatter on the comparisons of COVID with HIV. I’ve never been a fan of this, because there are so many unanswered questions. One thing I am sure of. Research shows the immune system does get damaged. It does. Which bits? How much? Recovery? What opportunistic infections? Impact on global disease patterns? Impact on animal disease patterns (ecology and food-chain threats)? All questions that will be answered over time. No-one should be surprised by this. It should not be even vaguely controversial. Plenty of viruses damage the immune system . We will find out exactly the extent of the nature of COVID on this aspect of health. Another thing I can say with some certainty. Your chances of recovery from a depressed post-viral immune system will not be improved by further [SARS-CoV-2] infections. I can see a lot of people directly comparing COVID with HIV. Rest assured. I am concerned. I just don’t find that particular comparison helpful. As many have already pointed out, there are significant differences too. You don’t walk into the supermarket and catch a new strain of HIV starting a whole new acute infection every 6-8 months, for example. But there are also signs that some immune cells are recovering many months after infection too – then again, there are probably reservoirs in the body that could potentially continue to mutate, and then cause other pathology down the line – as some animal coronaviruses do. I think COVID is quite an interesting and horrible disease. I expect we will see what repeated infections really do as time goes on. Excess deaths are already through the roof. One last attempt to clarify. Trying to make COVID into either a cold, or HIV, and ending up with “half-way between” – when in reality COVID is doing 100% COVID, which is turning out to be really, really bad in its own right… and it’s airborne… and we are catching it all the time. That’s the part I find frustrating with this comparison. SARS is a dangerous, dangerous disease. It always has been. Both of them [SARS-1 and SARS-2] . Yes, there are threads of similarities, and we can use our wealth of knowledge to extrapolate possible outcomes, and test treatments… But SARS is not half-way to anything. It is, in itself, a giant problem.”
by Rosichini et al / Journal of Allergy and Clinical Immunology
•
7 February 2023
❦ Lymphopenia , particularly when restricted to the T-cell compartment, has been described as one of the major clinical hallmarks in patients with coronavirus disease 2019 ( COVID-19 ) and proposed as an indicator of disease severity. Although several mechanisms fostering COVID-19-related lymphopenia have been described, including cell apoptosis and tissue homing, the underlying causes of the decline in T-cell count and function are still not completely understood. Patients with COVID-19 had reduced thymic function that was inversely associated with the severity of the disease. Our data demonstrate that the human thymus is a target of SARS-CoV-2 and thymic function is altered following infection . Note: Lymphopenia (also called lymphocytopenia) is a disorder in which your blood doesn't have enough white blood cells called lymphocytes. Lymphocytes play a protective role in your immune system. ❂ 📖 (7 Feb 2023 ~ Journal of Allergy and Clinical Immunology) SARS-CoV-2 infection of thymus induces loss of function that correlates with disease severity ➤ © 2023 Rosichini e t al / Journal of Allergy and Clinical Immunology.
by Emily Henderson ~ Medical Life Sciences / Tri Phan et al ~ Clinical Immunology
•
26 January 2023
❦ ‘Children have largely avoided severe COVID-19 symptoms because they have a strong initial ‘innate’ immune reaction that quickly defeats the virus. But unlike those of adults, children’s immune systems don’t remember the virus and don’t adapt, so when they’re next exposed to SARS-CoV-2, their body still treats it as a new threat. “Because children haven’t been exposed to many viruses, their immune system is still ‘naive’. And because they don't develop memory T cells, they are at risk of getting sick when they become reinfected. With each new infectious episode as they get older, there is a risk of their T cells becoming ‘exhausted’ and ineffective, like the T cells in older people. The price that children pay for being so good at getting rid of the virus in the first place is that they don’t have the opportunity to develop ‘adaptive’ memory to protect them the second time they are exposed to the virus,” says Professor Tri Phan.’ ❂ 📖 (26 Jan 2023 ~ Medical Life Sciences) Children's immune systems do not develop 'adaptive' memory to protect against second-time SARS-CoV-2 infection ➤ 📖 (January 2023 ~ Clinical Immunology) Tracking the clonal dynamics of SARS-CoV-2-specific T cells in children and adults with mild/asymptomatic COVID-19 ➤ © 2023 Emily Henderson / Medical Life Sciences.
by Emily Henderson / News Medical Life Sciences
•
12 January 2023
❦ Fungi such as Aspergillus are so common in our surroundings that we breathe in hundreds to thousands of spores every day. In healthy people, fungi typically pose no threat, but they can cause deadly infections in those with compromised immune systems. However, it is increasingly recognized that viral infections such as influenza or SARS-CoV-2 can increase the risk of invasive Aspergillus infections even in healthy people. ❂ 📖 (12 Jan 2023 ~ News-Medical.Net) New insights into deadly fungal invasion in people with compromised immune systems ➤ © 2023 Emily Henderson / News Medical Life Sciences.
by Terry Pender / Waterloo Region Record
•
20 December 2022
❦ Evolving research says COVID leaves many people at heightened risk for other infections. SARS-CoV-2 depletes the body’s supply of T-cells, * leaving young and old alike vulnerable to secondary infections. * (T-cells are the ‘front-line soldiers’ of the immune system, and the number of T-cells typically increases when the body is fighting off an infection.) “Individuals who are infected with COVID have many fewer T-cells – that’s a problem for us, because T-cells are a really important part of our immune system that helps defend us against infection.” But at least three studies show ✢ that COVID kills off a significant number of the body’s T-cells – so even when someone recovers from COVID, they are at a heightened risk for other viral, bacterial and fungal infections. “With the loss of these T-cells, we are now more vulnerable to all of these other infections, other viruses, other bacteria.” COVID-19 sparks what is called ‘programmed cell death’ among T-cells. Cells in the human body do this naturally as they age, but COVID-19 causes healthy T-cells to die that would otherwise be available to fight off infections. Many people who have had COVID brush it off, saying it was no worse than a bad case of the flu. What they don’t know is that they are more vulnerable to secondary infections that may cause them to seek help at a hospital emergency ward. ❂ ✢ 📖 (11 Jan 2023 ~ Nature Reviews / Immunology) Innate immune evasion strategies of SARS-CoV-2 ➤ 📖 (13 Jan 2023 ~ Preprint) Structure-based discovery of inhibitors of the SARS-CoV-2 Nsp14 N7-methyltransferase ➤ 📖 20 Apr 2021 ~ Nature / Cell Death & Differentiation) SARS-CoV-2 spike protein dictates syncytium-mediated lymphocyte elimination ➤ ❂ 📖 (20 Dec 2022 ~ Waterloo Region Record) Immune systems seriously weakened by COVID ➤ © 2022 Terry Pender / Waterloo Region Record.
by Davitt et al / Best Practice & Research Clinical Haematology
•
6 December 2022
❦ While COVID-19 was originally characterized as hyperinflammatory in its pathophysiology, emerging evidence demonstrates the possibility of a strongly immunosuppressive phenotype in more critical disease states. While immune activation from neutrophils and complement may contribute to inflammatory damage in the lungs, decreased antiviral responses, dysregulated macrophages and dendritic cells, and severe lymphopenia contribute to a suppressed state in which viral replication and secondary infections are prone. ❂ 📖 (6 Dec 2022 ~ Best Practice & Research Clinical Haematology) COVID-19 disease and immune dysregulation ➤ © 2022 Davitt et al / Best Practice & Research Clinical Haematology.
by Dr. Noor Bari, Emergency Medicine
•
30 November 2022
❦ “Lymphopenia is present during and after some viral infections, and this also varies between individuals. It is very transient in most cases, and by that I mean a couple of weeks. The viruses that cause longer derangement are already known to be associated with long-term immune system derangement – including secondary infections, immune amnesia and cancers. COVID-19 lymphopenia has been recorded present for months. COVID-19 has been found to destroy (engulf in syncytia), directly infect, stimulate, and suppress a lot of white-cell function. Reinfections are frequent. Secondary infections/reactivations observed. It’s a huge worry. As a general rule, efforts are made to control/treat viruses that cause prolonged immune system derangement. COVID-19 is wildly exceptional in that we are ignoring it, pretending the lymphocytes bounce back like after a cold, and are frequently infecting people with it. We are also losing naive lymphocytes in large numbers due to superantigen stimulation. This is very different to transient suppression of peripheral blood lymphocytes due to cytokines or migration. This is another example of people making assumptions (huge and wrong), based on entirely dissimilar pathogens. It’s very important to look at what happens in similar situations, such as post-other-super-antigen-carrying infections. (Nothing good.) I could have saved my energy today and just let everyone play with a super antigen and find out… but sadly, the people finding out the hardest lessons are not the people deciding to play with it. So… here we are…”
by Dr. Noor Bari, Emergency Medicine
•
10 November 2022
❦ “This morning someone said to me: — “I just can’t shake this... first a chest infection, and now a urine infection...” Someone else I know (very close) has had three eye infections post-COVID. Another has had a deterioration in their fertility, as compared to their baseline pre- and post-COVID. Measured. It’s almost as if the stuff in the science papers is real. None of them have twigged that COVID might have toasted them yet either. They are all heading into this next wave with no idea how dangerous it might be to abuse their already struggling immune system like this. You know what’s coming next... Multi-drug-resistant bacteria. Many are already here, but this is going to get really out of control. Trying to treat infections in immunodeficient patients is a great way to make loads of drug-resistant bacteria and viruses.” ✾ 📖 (24 Sep 2025 ~ CIDRAP/University of Minnesota) Outpatient antibiotic use in COVID patients linked to 'downstream' antibiotic resistance ➤ 📖 (15 Jul 2025 ~ UKHSA: News story) UTIs [Urinary Tract Infections] cost NHS hospitals over £600m last year ➤ 📖 (26 Jun 2025 ~ Forbes) Cancer Patients Face Silent Crisis From Superbugs, New Research Shows ➤ 📖 (12 Dec 2024 ~ CIDRAP/University of Minnesota) Report describes spread of highly drug-resistant cholera strain ➤ 📖 (1 Nov 2024 ~ China CDC Weekly) Emergence of a New Sublineage of Candida auris Causing Nosocomial Transmissions - Beijing Municipality, China, March-September 2023 ➤ 📖 (17 May 2024 ~ CIDRAP/University of Minnesota) Global Meta-analysis estimates 43% rate of multidrug resistance in COVID patients ➤ 📖 (14 May 2024 ~ Journal of Infection) Global antimicrobial resistance and antibiotic use in COVID-19 patients within health facilities: A systematic review and meta-analysis of aggregated participant data ➤ 📖 (24 May 2023 ~ Current Microbiology) Interaction Between SARS-CoV-2 and Pathogenic Bacteria ➤ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ 📖 (29 Mar 2023 ~ Journal of Fungi) Fungal-Bacterial Co-Infections and Super-Infections among Hospitalized COVID-19 Patients: A Systematic Review ➤ 📖 (30 Sep 2021 ~ Business Insider) Drug-resistant infections in the US have risen sharply during the pandemic, and experts warn it's getting worse as COVID patients overwhelm hospital resources ➤
by Dr. Noor Bari, Emergency Medicine
•
30 October 2022
❦ “COVID-19 is fighting back by generally depressing the whole adaptive immune system. We are showing narrow resilience to COVID reinfections due to adapting – but we are becoming more vulnerable in general to infections of all kinds. ❦ Worst case scenario A single infection causes on-going and progressive immunodeficiency . ❦ Best case scenario A single infection causes temporary immunosuppression , and we suppress COVID transmission enough to allow recovery. ❦ Most likely scenario, medium-term Immunosuppression that becomes continuous and possibly progressive due to reinfections. Reduced immune function after a viral infection is not unusual. Many viruses do this. The concerning issue is the length and breadth of the immune system dysfunction, coupled with emerging evidence of other pathogens taking advantage .” ✾ ❦ Immunosuppression ~ Suppression of the immune system and its ability to fight infection. ❦ Immunodeficiency ~ A state in which the immune system’s ability to fight infectious diseases and cancer is compromised, or entirely absent.
by Dr. Lisa Iannattone, Assistant Professor of Dermatology
•
15 October 2022
❦ “Not catching a common virus for a year or two, or five, does not make you respond to it like an immunosuppressed person the next time you catch it. Avoiding pathogens doesn’t damage your immune system. On the other hand, there are many pathogens out there that are capable of damaging your immune system. Pathogens are foes, not friends.”
by Dr. Lisa Iannattone, Assistant Professor of Dermatology
•
1 October 2022
❦ “Immunity debt” is making the rounds again. So here’s my reminder that while there are viruses that are more severe if caught as a teen or adult (like polio or chickenpox), that isn’t the case for respiratory viruses . There’s a mortality benefit from first RSV and flu infections being delayed. So no, your toddler doesn’t need to catch all the viruses before the age of two to “build their immune system”. In fact, it’s the opposite: infants and young toddlers are more at risk of hospitalization and death from many respiratory viruses at their age than older children. You know how we’re asked not to give kids honey until they’re one? Or how Health Canada has a whole list of unsafe foods for kids under five? “ For many pathogens, kids are more susceptible to severe outcomes when they’re very young. ” And there is benefit to delaying exposure. This new (and very politically convenient) idea that it’s always best to catch pathogens very early in life “to build your immune system” can actually be quite dangerous when you take the time to think it all the way through. Stop blindly promoting “immunity debt” pseudoscience. Three years ago, I never would have believed that I’d one day see scientists and MDs [medical doctors] promoting the idea that it’s good for infants and young toddlers to be exposed to dangerous respiratory viruses like flu and RSV, instead of trying to delay those first infections – and yet here we are.”
by Hayley Muendlein / The Conversation
•
17 August 2022
❦ The 1918 influenza pandemic resulted in the loss of over 3% of the world’s population – at least 50 million people. But it wasn’t the flu virus that caused the majority of these deaths. An analysis of lung samples collected during that flu pandemic indicated that most of the deaths were likely due to bacterial pneumonia , which ran rampant in the absence of antibiotics. Even in more recent history, like the 1957 H2N2 and 2009 H1N1 flu pandemics , nearly 18% of patients with viral pneumonia had additional bacterial infections that increased their risk of death. And the COVID-19 pandemic is no different. ❂ 📖 (17 Aug 2022 ~ The Conversation) When COVID-19 or flu viruses kill, they often have an accomplice – bacterial infections ➤ © 2022 Hayley Muendlein / The Conversation.
by Dr. Noor Bari, Emergency Medicine
•
21 July 2022
❦ “So, we want to “live with the virus”. Is there any evidence of this occurring successfully anywhere? Yes! In bats... and it has taken 64 million years of evolution to get there. To “live with the virus”, bats have better host defences – they don’t overdo inflammation, and they can get rid of toxic compounds and deal with reactive oxygen species much better than humans. They literally live with the virus .
by Liz Szabo / KFF Health News
•
4 March 2021
❦ While all viruses find ways to evade the body’s defenses, a growing field of research suggests that the coronavirus unhinges the immune system more profoundly than previously realized. Some Covid survivors have developed serious autoimmune diseases, which occur when an overactive immune system attacks the patient, rather than the virus. Doctors in Italy first noticed a pattern in March 2020, when several Covid patients developed Guillain-Barré syndrome, in which the immune systems attacks nerves throughout the body, causing muscle weakness or paralysis. As the pandemic has surged around the world, doctors have diagnosed patients with rare, immune-related bleeding disorders. Other patients have developed the opposite problem, suffering blood clots that can lead to stroke. All these conditions can be triggered by autoantibodies – rogue antibodies that target the patient’s own proteins and cells. ❂ 📖 (4 Mar 2021 ~ KFF Health News) Coronavirus Deranges the Immune System in Complex and Deadly Ways ➤ © 2021 Liz Szabo / KFF Health News.
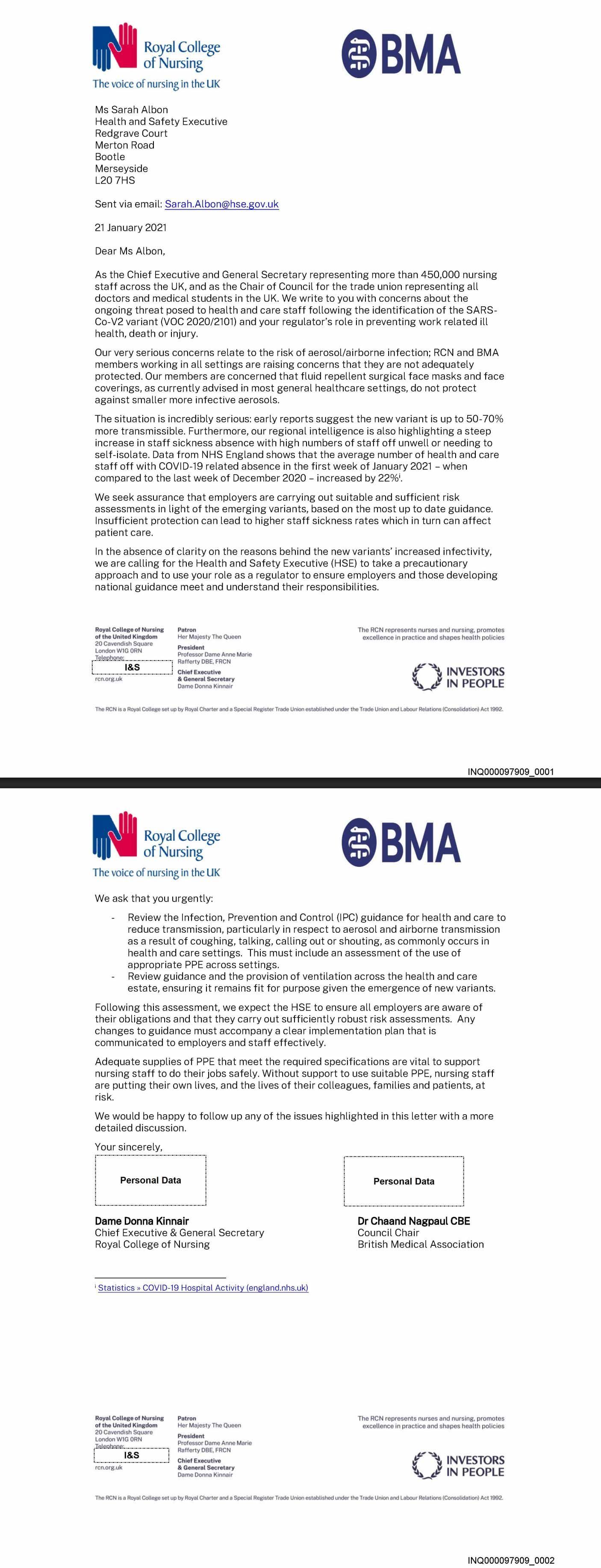
by The Royal College of Nursing (RCN/UK) and The British Medical Association (BMA)
•
21 January 2021
‘Our very serious concerns relate to the risk of aerosol/airborne infection; RCN and BMA members working in all settings are raising concerns that they are not adequately protected. Our members are concerned that fluid-repellent surgical face masks [FRSM] and face coverings, as currently advised in most general healthcare settings, do not protect against smaller more infective aerosols. ’
by Dr. Michael Lin, MD PhD
•
2 April 2020
❦ “I am realizing more and more how unusual, unscientific, unmedical, and counterproductive it is for the World Health Organization (WHO) to select the name COVID-19 and reject SARS2. In fact it would be most consistent with medical practice to just call it SARS. Here’s why. In 1981, cases of immunodeficiency emerged in San Francisco; in 1982 , the Centers for Disease Control and Prevention ( CDC ) named this disease acquired immunodeficiency syndrome ( AIDS ). No agent was known at the time... Compare : in 2002 , cases of atypical non-bacterial pneumonia appeared in Guandong; in 2003 the CDC named this severe acute respiratory syndrome ( SARS ). No agent was known at the time... In 1983 , the virus that causes AIDS was discovered by Françoise Barré-Sinoussi and Luc Montaignier. It was eventually named HIV in 1986 by the International Committee on the Taxonomy of Viruses ( ICTV ). Compare : in 2003 , the virus that causes SARS was isolated in Hong Kong, sequenced by the CDC and a Canadian consortium. It was named SARSCoV in 2004 by the ICTV. ➲ Taxon Details for Severe acute respiratory syndrome-related coronavirus ➤ In 1986 , a milder acquired immunodeficiency syndrome was discovered in West Africa, and the virus was quickly isolated by the Montaignier group. It had 50% sequence identity to HIV . The virus was named HIV-2 . The disease name ? Unchanged: AIDS . Compare : In 2019 , a severe acute respiratory distress syndrome was discovered in Wuhan and the virus was quickly isolated by Wuhan scientists. It had 79% sequence identity to SARSCoV . The virus was named SARSCoV-2 by the ICTV. The disease name ? Well, that’s when the WHO stepped in. To review: HIV-1 and HIV-2 are 50% identical , and both cause immunodeficiency . They result in different disease severities (you’re less likely to die from HIV-2) – but the diseases they cause are (or the disease they cause is) considered the same : AIDS . SARSCoV-1 and SARSCoV-2 are 79% identical , and both cause severe acute respiratory distress . They result in different disease severities (you’re less likely to die from SARSCoV-2), so by analogy to HIV-1/2→AIDS , the diseases they cause should be considered the same : SARS . However, the WHO stepped in (why does the CDC have to defer to them anyway?) and decided that the one requirement for the name was that it not mention SARS . Thus the terrible name COVID-19 was chosen. It stands for coronavirus disease , and thus has no useful medical information . It is an open suspicion that this was done to deflect criticism for a slow response to what is basically a second SARS epidemic . Because we already knew how to stop [the airborne] SARSCoV – and knew that it was bad – there was no excuse for not quickly addressing what is basically a strain of SARSCoV . The purposeful hiding of the identity of the COVID-19 virus – that it is a strain of SARS virus – has had severe negative consequences to world health . By not realizing that we are dealing with SARS, many political leaders have failed to address the epidemic forcefully enough. Also, the term COVID-19 hinders clinical education and communication . Let’s compare to AIDS again. Calling the disease(s) caused by HIV-1 and HIV-2 as AIDS in both cases has clinical utility . The signs and symptoms are similar enough that it helps to consider HIV-1/2 together . Considering HIV-1/2 together also reminds us that treatments and preventive steps we learn from one can be used on the other . Likewise, COVID-19 should have been called SARS , SARS2 , or – as a compromise – variably severe acute respiratory syndrome , vSARS . Li Wenliang , who warned about the new outbreak in Wuhan, had it exactly right : “Seven confirmed cases of SARS were reported... The latest news is, it has been confirmed that they are coronavirus infections , but the exact virus strain is being subtyped.” Disease names have always been guided by a desire to inform . The WHO has taken the opposite approach , to misinform . Not surprisingly, confusion has resulted. With millions dying , we are now seeing the tragic consequences of WHO’s placement of politics over medicine and science . Since some people seem to have already forgotten their history (or maybe were living under a rock when the WHO naming decision happened), here’s the quote from the WHO itself...” ✾ ❦ From Science , 12 Feb 2020 : “COVID-19. I’ll spell it: C-O-V-I-D hyphen one nine. COVID-19.” ‘That’s how Tedros Adhanom Ghebreyesus, head of the World Health Organization (WHO), introduced the agency’s official name for the new disease that’s paralyzing China and threatening the rest of the world. The Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses, the paper noted, had decided that the virus is a variant of the coronavirus that caused an outbreak of severe acute respiratory syndrome (SARS) in 2002–03. So, it named the new pathogen severe acute respiratory syndrome-related coronavirus 2 , or SARS-CoV-2 . But that’s not a name WHO is happy with , and the agency isn’t planning on adopting it. “From a risk communications perspective , using the name SARS can have unintended consequences in terms of creating unnecessary fear for some populations, especially in Asia which was worst affected by the SARS outbreak in 2003,” a WHO spokesperson wrote in an email to Science . “ For that reason and others , in public communications WHO will refer to ‘the virus responsible for COVID-19’ or ‘the COVID-19 virus , ’ but neither of these designations is intended as replacements for the official name of the virus” that the study group has picked. Misunderstandings about the virus and disease names began almost immediately ...’ 📖 (12 Feb 2020 ~ Science) Update: ‘A bit chaotic.’ Christening of new coronavirus and its disease name create confusion ➤ ✾ ❦ From the WHO Director-General’s mouth on 11 Feb 2020 : — “First of all, we now have a name for the disease: COVID-19. I’ll spell it: C-O-V-I-D hyphen one nine – COVID-19. Under agreed guidelines between WHO, the World Organisation for Animal Health and the Food and Agriculture Organization of the United Nations, we had to find a name that did not refer to a geographical location, an animal, an individual or group of people, and which is also pronounceable and related to the disease .” [Ed: So ‘ SARS ’ would’ve worked, then.] “Having a name matters to prevent the use of other names that can be inaccurate or stigmatizing. It also gives us a standard format to use for any future coronavirus outbreaks ...” 📖 (11 Feb 2020 ~ World Health Organization) WHO Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020 ➤ ❂ © 2020 by Dr. Michael Lin, MD PhD ➲
by Dr. Noor Bari, Emergency Medicine
•
18 April 2025
“We are drunk-driving in healthcare... with a pathogen that has a 10% fatality rate in that setting.”
by Dr. Noor Bari, Emergency Medicine ❂ NextStrain.org
•
29 October 2024
❦ “If you are letting yourself get infected and taking no precautions against passing it on, you are not a passive bystander for your next infection. You’ve participated in creating it.”
by Dr. Noor Bari, Emergency Medicine
•
30 August 2023
❦ “It’s not like I’ve never seen people die of causes that are a result of their lifestyle... but it’s awful seeing people die as a result of other people’s lifestyles... and now that includes their healthcare provider! It feels very similar to watching people die from another person’s drunk-driving... That’s the closest similar situation I can think of. We are drunk-driving in healthcare... with a pathogen that has a 10% fatality rate in that setting.”
by Dr. Noor Bari, Emergency Medicine
•
27 August 2023
❦ “If y’all are busy weakening your immune systems with one virus, let me assure you that there are packs of other pathogens out there waiting to chew on the leftovers.”
by Dr. Noor Bari, Emergency Medicine
•
11 August 2023
❦ “Anything that is more transmissible will kill in two ways. Infecting more people. Worsening pressure on healthcare.”
by Dr. Noor Bari, Emergency Medicine
•
8 August 2023
❦ “In real life, no-one… and I mean no-one… is actually living a normal life if they have abandoned C-19 precautions. Either they are suffering the effects of illness themselves, are caring for someone that is sick, grieving, or all of the above. It’s not all people of one race/genotype either. It’s across a broad spectrum of people. It’s not even segregated by money. People with money that did not take it seriously enough to seek treatment have also fallen foul of problems. At this point in my social world the denial is being peeled away… and people are opening up about issues. However many still feel unable to prevent further problems. I’m seeing everything from acute COVID deaths to long COVID deaths. Every kind of autoimmune disease seems to be on the cards, colitis, hearing loss, joint problems… One common thread… people either have not made the connection to C-19, or think they are the odd one out. That they have somehow personally failed to be tough enough to weather the SARS storm. One can only congratulate the ghouls that have allowed that feeling to spread. I mean no-one I know… So all these people that I see on-and-off are living in their own quiet bubble of difficulty… and no-one is brave enough to tackle anything because no-one wants to be different… or perceived as a failure… or in many cases, they don’t know what to do anyway… This is a massive failure of public health. The anti-maskers are out on social media, loud and proud; public health departments barely whisper some diluted numbers once a week. Literally, things tick along “normally” in the conversation until you hit that bump. Ever since my last infection I _____. Fill in the blank. It’s often something that sounds really minor… but those that have read the data know what it really means. Quit the gym. Food is bland. Ringing in ears. Headaches. Joint pain. Stomach upset. Dizzy. Heart races. Tired. Stopped driving or stopped driving long distances. Quit the booze. Rashes. Keep getting xyz infections. Just going to tack on here that the first sentence contains an omission. “Real life” = People I know in real life. My real-life home village is sick or grieving or caring. Pretty much every household.”
by Dr. Noor Bari, Emergency Medicine
•
16 June 2023
❦ “Dear economy enthusiasts... The only humane way to avoid locking down for airborne disease control ever again is to set up safer indoor-air infrastructure... globally. Everyone that is slowing down this process is asking for another lockdown. Or mass murder. More likely another lockdown though because in the end, if bird flu takes off or MERS has an interesting offspring... the public will not stomach as much death as the anti-lockdown and dirty-air proponents would like.”
by Dr. Noor Bari, Emergency Medicine
•
27 May 2023
❦ “There is no such thing as “personal risk assessment” for the vast majority of people. A tiny number of dominant personalities in your life (and it could be you) have decided what to do, and the rest will follow. Even those that are making the decisions are not making a personal risk assessment. They are making a group risk assessment and taking their whole family/community with them. People may not even realise this – that they have made the decision on behalf of their entire household/class/company... but they have... If there is no responsible public health leadership, someone else is leading... because that is how we work, by and large, as a species. Someone is in charge... someone is always in charge, and unfortunately... misinformation is rife.”
by Dr. Noor Bari, Emergency Medicine
•
26 May 2023
❦ “No-one said life was gonna be easy. No-one said living through a pandemic was going to be easy. It’s all about what you think is important and worth fighting for. I chose health, lives, and sticking together. I chose to try to solve problems, not hide them. You can rewrite history. You can say that the mass overseas graves didn’t matter. You can say that we didn’t need to lock down in Australia in 2020 (when we had no PPE, no vaccines, and no therapeutics). I know different. I was there. Shed enough tears, attended enough zoom funerals… I know it wasn’t easy. I saw the tears when I said that a family on the breadline needed to isolate. I saw the heartbreak as I led a person away from their family, across the red line into the “red zone”. Even as I walked away from my family every day into the red zone, I felt your effort with me. When I said goodbye to my kid every day, and isolated away from my family to protect them from any accidental breaches... I know you all sacrificed too... ...and I was so grateful, and so proud... I wasn’t the one saving lives, you all were. You saved my life... I’m sure of it. We didn’t have enough PPE... Don’t ever forget that, and don’t let those bombastic characters writing rubbish articles about lockdown ever take that away from you.”
by Dr. Noor Bari, Emergency Medicine
•
20 February 2023
❦ “I’m vaguely following the chatter on the comparisons of COVID with HIV. I’ve never been a fan of this, because there are so many unanswered questions. One thing I am sure of. Research shows the immune system does get damaged. It does. Which bits? How much? Recovery? What opportunistic infections? Impact on global disease patterns? Impact on animal disease patterns (ecology and food-chain threats)? All questions that will be answered over time. No-one should be surprised by this. It should not be even vaguely controversial. Plenty of viruses damage the immune system . We will find out exactly the extent of the nature of COVID on this aspect of health. Another thing I can say with some certainty. Your chances of recovery from a depressed post-viral immune system will not be improved by further [SARS-CoV-2] infections. I can see a lot of people directly comparing COVID with HIV. Rest assured. I am concerned. I just don’t find that particular comparison helpful. As many have already pointed out, there are significant differences too. You don’t walk into the supermarket and catch a new strain of HIV starting a whole new acute infection every 6-8 months, for example. But there are also signs that some immune cells are recovering many months after infection too – then again, there are probably reservoirs in the body that could potentially continue to mutate, and then cause other pathology down the line – as some animal coronaviruses do. I think COVID is quite an interesting and horrible disease. I expect we will see what repeated infections really do as time goes on. Excess deaths are already through the roof. One last attempt to clarify. Trying to make COVID into either a cold, or HIV, and ending up with “half-way between” – when in reality COVID is doing 100% COVID, which is turning out to be really, really bad in its own right… and it’s airborne… and we are catching it all the time. That’s the part I find frustrating with this comparison. SARS is a dangerous, dangerous disease. It always has been. Both of them [SARS-1 and SARS-2] . Yes, there are threads of similarities, and we can use our wealth of knowledge to extrapolate possible outcomes, and test treatments… But SARS is not half-way to anything. It is, in itself, a giant problem.”
by Dr. Noor Bari, Emergency Medicine
•
22 January 2023
❦ “No. We haven’t gone back to normal. We have gone forward into abnormal. Really abnormal. Kill your elders abnormal. Douse the kids in viruses abnormal. Ignore and kill disabled people abnormal. Please go back to normal... because I don’t believe for a second that when you wake up and look in the mirror, that this is what you ever wanted to see looking back at you. It’s not too late.”
by Dr. Noor Bari, Emergency Medicine
•
4 January 2023
❦ — “How was your New Year?” — “S’ok...” Sad face... young adult person... “I got sick... kind of like a cold...” (But face says, “It ruined my New Year.”) So much is left unsaid. So many assumptions that everyone else is having fun – why not me? Guilt about being a let-down. (‘Am I not strong enough? My immunity not good enough?’) Others move on to chat about dining out at restaurants... This young person turns away, and continues to work. Isolated in her thoughts... How desperately I wanted to go over to her and say, “You are not alone...” But I’m a stranger, just passing... I think about how people in power are misleading and hurting young people. It’s deplorable.
by Dr. Noor Bari, Emergency Medicine
•
30 December 2022
❦ “COVID-19 causes lung fibrosis. It affects the immune system, and it causes liver fibrosis . COVID-19 causes brain inflammation and heart inflammation, strokes, heart attacks and large blood clots. COVID-19 causes diabetes . COVID-19 can cause kidney failure. I could go on... and on. Bone necrosis, joint pain, hair and teeth falling out. Do you normally expect a cold to make your teeth fall out ? Look up ‘lung fibrosis’ and ‘liver fibrosis’. Google them, and read about the complications. Read how patients that have these progressive diseases die. (Apologies to patients that already know.) Time and again, these patients have said to me (particularly when I was a young medical student): “Don’t do what I did.” “Don’t smoke.” “Alcohol is...” “I wish I had never...” “Save yourself...” Of those dying of infectious causes of lung and liver fibrosis: “Why me...?” “I wish I could have avoided that infection...” Stop. Stop as many COVID infections as you can. Stop now. Now is your chance to avoid treading these terrible paths. Once COVID has weakened your organs and immune system, every other pathogen – and even some environmental/commensal bugs – can move in... You will feel nothing wrong, nothing wrong, nothing wrong... then... the cascade of deterioration will snowball. Stop now while you are still in the “I feel nothing wrong” phase. There may well already be stuff wrong, but it’s better to try to stay in this phase than accelerate towards death any faster than is avoidable. No, not everyone will get every effect to the same extent, but macrophages do get activated by COVID (as well as other immune pathways and cells). Some of the inflammation in the body has been observed for months. That is a recipe for damage and fibrosis. I wrote this after hearing – again and again – “I have a cough, it just won’t budge, and it’s not COVID”. I don’t know what's causing all the coughing. Could be anything... but this is one of the ways I would expect widespread prevalence of lung damage to present. It’s also one of the ways I would expect chronic infections with slow-growing pathogens (like TB or atypical pneumonias) to present... Chronic coughs can also have other malignant or serious causes. These should be assessed and monitored by a GP if it’s not budging. Please... try to look after yourselves.. .”
by Dr. Noor Bari, Emergency Medicine
•
30 November 2022
❦ “Lymphopenia is present during and after some viral infections, and this also varies between individuals. It is very transient in most cases, and by that I mean a couple of weeks. The viruses that cause longer derangement are already known to be associated with long-term immune system derangement – including secondary infections, immune amnesia and cancers. COVID-19 lymphopenia has been recorded present for months. COVID-19 has been found to destroy (engulf in syncytia), directly infect, stimulate, and suppress a lot of white-cell function. Reinfections are frequent. Secondary infections/reactivations observed. It’s a huge worry. As a general rule, efforts are made to control/treat viruses that cause prolonged immune system derangement. COVID-19 is wildly exceptional in that we are ignoring it, pretending the lymphocytes bounce back like after a cold, and are frequently infecting people with it. We are also losing naive lymphocytes in large numbers due to superantigen stimulation. This is very different to transient suppression of peripheral blood lymphocytes due to cytokines or migration. This is another example of people making assumptions (huge and wrong), based on entirely dissimilar pathogens. It’s very important to look at what happens in similar situations, such as post-other-super-antigen-carrying infections. (Nothing good.) I could have saved my energy today and just let everyone play with a super antigen and find out… but sadly, the people finding out the hardest lessons are not the people deciding to play with it. So… here we are…”
by Dr. Noor Bari, Emergency Medicine
•
21 November 2022
❦ “This is quite possibly the most absurd thing you will read today. Let’s take this one step at a time. For the purposes of this short essay, I will be ‘vulnerable’.”
by Dr. Noor Bari, Emergency Medicine
•
10 November 2022
❦ “This morning someone said to me: — “I just can’t shake this... first a chest infection, and now a urine infection...” Someone else I know (very close) has had three eye infections post-COVID. Another has had a deterioration in their fertility, as compared to their baseline pre- and post-COVID. Measured. It’s almost as if the stuff in the science papers is real. None of them have twigged that COVID might have toasted them yet either. They are all heading into this next wave with no idea how dangerous it might be to abuse their already struggling immune system like this. You know what’s coming next... Multi-drug-resistant bacteria. Many are already here, but this is going to get really out of control. Trying to treat infections in immunodeficient patients is a great way to make loads of drug-resistant bacteria and viruses.” ✾ 📖 (24 Sep 2025 ~ CIDRAP/University of Minnesota) Outpatient antibiotic use in COVID patients linked to 'downstream' antibiotic resistance ➤ 📖 (15 Jul 2025 ~ UKHSA: News story) UTIs [Urinary Tract Infections] cost NHS hospitals over £600m last year ➤ 📖 (26 Jun 2025 ~ Forbes) Cancer Patients Face Silent Crisis From Superbugs, New Research Shows ➤ 📖 (12 Dec 2024 ~ CIDRAP/University of Minnesota) Report describes spread of highly drug-resistant cholera strain ➤ 📖 (1 Nov 2024 ~ China CDC Weekly) Emergence of a New Sublineage of Candida auris Causing Nosocomial Transmissions - Beijing Municipality, China, March-September 2023 ➤ 📖 (17 May 2024 ~ CIDRAP/University of Minnesota) Global Meta-analysis estimates 43% rate of multidrug resistance in COVID patients ➤ 📖 (14 May 2024 ~ Journal of Infection) Global antimicrobial resistance and antibiotic use in COVID-19 patients within health facilities: A systematic review and meta-analysis of aggregated participant data ➤ 📖 (24 May 2023 ~ Current Microbiology) Interaction Between SARS-CoV-2 and Pathogenic Bacteria ➤ 📖 (18 Apr 2023 ~ BMC Infectious Diseases) Fungal infection profile in critically ill COVID-19 patients: a prospective study at a large teaching hospital in a middle-income country ➤ 📖 (29 Mar 2023 ~ Journal of Fungi) Fungal-Bacterial Co-Infections and Super-Infections among Hospitalized COVID-19 Patients: A Systematic Review ➤ 📖 (30 Sep 2021 ~ Business Insider) Drug-resistant infections in the US have risen sharply during the pandemic, and experts warn it's getting worse as COVID patients overwhelm hospital resources ➤
by Dr. Noor Bari, Emergency Medicine
•
6 November 2022
❦ “During my young and ‘indestructible’ days, I did a lot of risky things. I now have a dodgy ankle, and various other aches and pains to remind me... Young people these days will also accumulate their scars of youth... but in my opinion, the COVID scars were unnecessary. We could have made it so much safer to travel and have fun by controlling disease properly. We gave up on them, our youth. We left them last for vaccines, and last for any consideration of their needs. They can’t even date properly without excess risk of long-term health problems because we can’t be bothered to do the work. Dating and finding a partner is a need , by the way. Sure, there are ways around this… but realistically, zero COVID would have been for them. The young. People think it’s to protect the old... but that’s only a small part of the story! Zero COVID would have given our kids safer schools. Parties would be safer. Sport would be safer, and they could excel without fear of COVID ruining their goals. We should have done it for the kids. See what I mean. We have misguided and abandoned them.”
by Dr. Noor Bari, Emergency Medicine
•
6 November 2022
❦ “What are we going to tell young men in twenty years’ time if they discover that they can’t ever have an erection in the usual manner due to repeated childhood COVID infections? Have we thought about using vaccines and therapeutics in children to prevent this? What about protecting children with NPIs ( non-pharmaceutical interventions )? We all worry about kids missing out on fun stuff in this pandemic. What about their sexual health later in life? Is this not fun? Is this not important? Is this not for them ? Let’s not be squeamish. Let’s think this through properly. Our youth are being repeatedly infected with a pathogen that we know affects sexual and reproductive health in a myriad of ways. Due to the fact that I will likely be dead by the time you figure this out, I’m going to take the liberty of saying a few things now. 1) This is unacceptable. 2) I told you so. 3) I’m sorry future adults, I really tried. I hope that solutions come your way.”
by Dr. Noor Bari, Emergency Medicine
•
30 October 2022
❦ “COVID-19 is fighting back by generally depressing the whole adaptive immune system. We are showing narrow resilience to COVID reinfections due to adapting – but we are becoming more vulnerable in general to infections of all kinds. ❦ Worst case scenario A single infection causes on-going and progressive immunodeficiency . ❦ Best case scenario A single infection causes temporary immunosuppression , and we suppress COVID transmission enough to allow recovery. ❦ Most likely scenario, medium-term Immunosuppression that becomes continuous and possibly progressive due to reinfections. Reduced immune function after a viral infection is not unusual. Many viruses do this. The concerning issue is the length and breadth of the immune system dysfunction, coupled with emerging evidence of other pathogens taking advantage .” ✾ ❦ Immunosuppression ~ Suppression of the immune system and its ability to fight infection. ❦ Immunodeficiency ~ A state in which the immune system’s ability to fight infectious diseases and cancer is compromised, or entirely absent.
by Dr. Noor Bari, Emergency Medicine
•
28 July 2022
❦ “I graduated from UCL. It has changed a lot since I was there. The ability to prioritise actions in an emergency is my job. You have to do things in the right order, or none of it works. We need COVID control, so we can free up resources to do other work. I don’t just mean health resources either. Depletion of workers due to sick leave; long-term illness; carer duties; and death – with some jobs becoming frankly undesirable. The expected benefits of ventilation and masks in essential services would be to reduce Reff * and save lives. * Reff , or the effective transmission number , is a measure used to indicate how many people, on average, a single infected person will transmit a disease to. A Reff value above 1 suggests that the infection is spreading , while a value below 1 indicates that the outbreak is declining . How much… you have to do it to find out, because it hasn’t been done before. We have to build this plane while flying. No room for excess baggage. Small case studies (like individual schools, or wards in a hospital ) indicate the benefit might be quite a lot. Even if it’s not as much as hoped, it has to be done, because we are rapidly accumulating long-term sickness. We have to try everything to slow that process.”
by Dr. Noor Bari, Emergency Medicine
•
21 July 2022
❦ “So, we want to “live with the virus”. Is there any evidence of this occurring successfully anywhere? Yes! In bats... and it has taken 64 million years of evolution to get there. To “live with the virus”, bats have better host defences – they don’t overdo inflammation, and they can get rid of toxic compounds and deal with reactive oxygen species much better than humans. They literally live with the virus .
by Dr. Noor Bari, Emergency Medicine
•
9 April 2022
❦ “I think it would be good if people stop asking family members of vulnerable people when they will unmask and go on holiday… and what their off-ramp is. Like… is “off-ramp” code for bumping off the vulnerable person in the household? Exit strategy via coffin? The faster everyone accepts that some of us can’t even go to a dentist without a risk-benefit analysis, let alone a dinner party, the happier we will all be. Do I walk around asking you about your personal choice not to mask? What makes you think you can ask me why I do mask? I know that tone says you aren’t actually interested in the answer. Let it go. No, no… I don’t have to learn to “live my life again”. I am living my life the way I have always lived my life. With due respect for myself and others.”
by Dr. Noor Bari, Emergency Medicine
•
20 December 2021
❦ “Let’s play pretend. Pretend we have unlimited resources to staff the hospitals. Unlimited ICU beds. We let COVID-19 take its natural course. COVID-19 would average, what? Two or three infections per person, per year? Let’s be conservative. Let’s say you get COVID-19 once a year. So once a year, a certain proportion of all human beings, except those in countries with good COVID control will: die; have reproductive difficulties like erectile dysfunction; get heart failure; lose the pleasure of the smell and taste of food; have new autoimmune issues; develop new cognitive issues; have vascular problems like strokes; suffer other organ damage, like kidney failure; receive a new diagnosis of diabetes. Etc. Each of these has a percentage prevalence in cases. Some of those numbers are not small. Each time, there will be people that get one or more of these issues. Each of those conditions has their own associated increase in mortality. Then there is the drop in productivity and quality of life. How long do you think it would be before the majority of the population has something not quite right with them due to COVID-19? I don’t think it would take all that long. Ten years maybe? Twenty? How can it possibly be a sane public health strategy to have hospitalisation and ICU capacity preservation as the goal of a nation, when the obvious and massive loss of health (and life) due to circulating COVID can be predicted already? Some years, we will not have a great match between vaccines and circulating strains (such as Omicron); other years we will get it right (maybe if we are fast enough, and we aren’t yet). What does that mean? There will be multiple episodes in the future where vaccine-mediated cover and infection-mediated immunity will not be great. That means the organ damage will be somewhat more severe. Why are public health officials OK with this? Even if we can never get back to zero COVID, why are they OK with having a high frequency of infections per lifetime? Am I in an alternate universe where I can see these studies and they can’t? We have therapeutics coming in, so that will help, but they aren’t 100% magic bullets either. People need a combination of factors to bounce through a COVID infection without noticeable effects (although kidney damage can present late). That combination, to be maintained at all times for an individual is difficult, let alone a population. The strategy of “Living with COVID-19” is fatally flawed. That flaw is the fact that COVID-19 is a rapidly mutating virus that causes irreversible, or slowly reversible damage to the human body. We can’t actually withstand it for our usual natural lifetimes. The government must show the modelling for long-term health outcomes for their “living with the virus” plans. The economic impact of the same. All the colleges of medicine should submit their modelling on how COVID-19 is affecting human health. This is critically important work. How a biohazard was allowed into Australia and allowed to circulate – without modelling its overall impact on human health – is a matter that should be investigated thoroughly. It was a huge decision. There should have been expert discussion and documentation. No… Saying “We didn’t know” is not good enough. If you don’t know… Don’t play with SARS.”