📖 Beyond breathing: How COVID-19 affects your heart, brain and other organs
“I would argue that COVID-19 is not a disease of the lungs at all.
It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system.”
📖 (16 Jan 2024 ~ American Heart Association) ‘Beyond breathing: How COVID-19 affects your heart, brain and other organs’.
❦ Scientific Media Article ~ ‘Beyond breathing: How COVID-19 affects your heart, brain and other organs’
By Michael Merschel / American Heart Association (16 Jan 2024)
❦ ‘The (2023-2024) New Year started with an increase in COVID-19 hospitalizations in the U.S., prompting Hernandez and other experts to advise caution, especially for those at high risk.
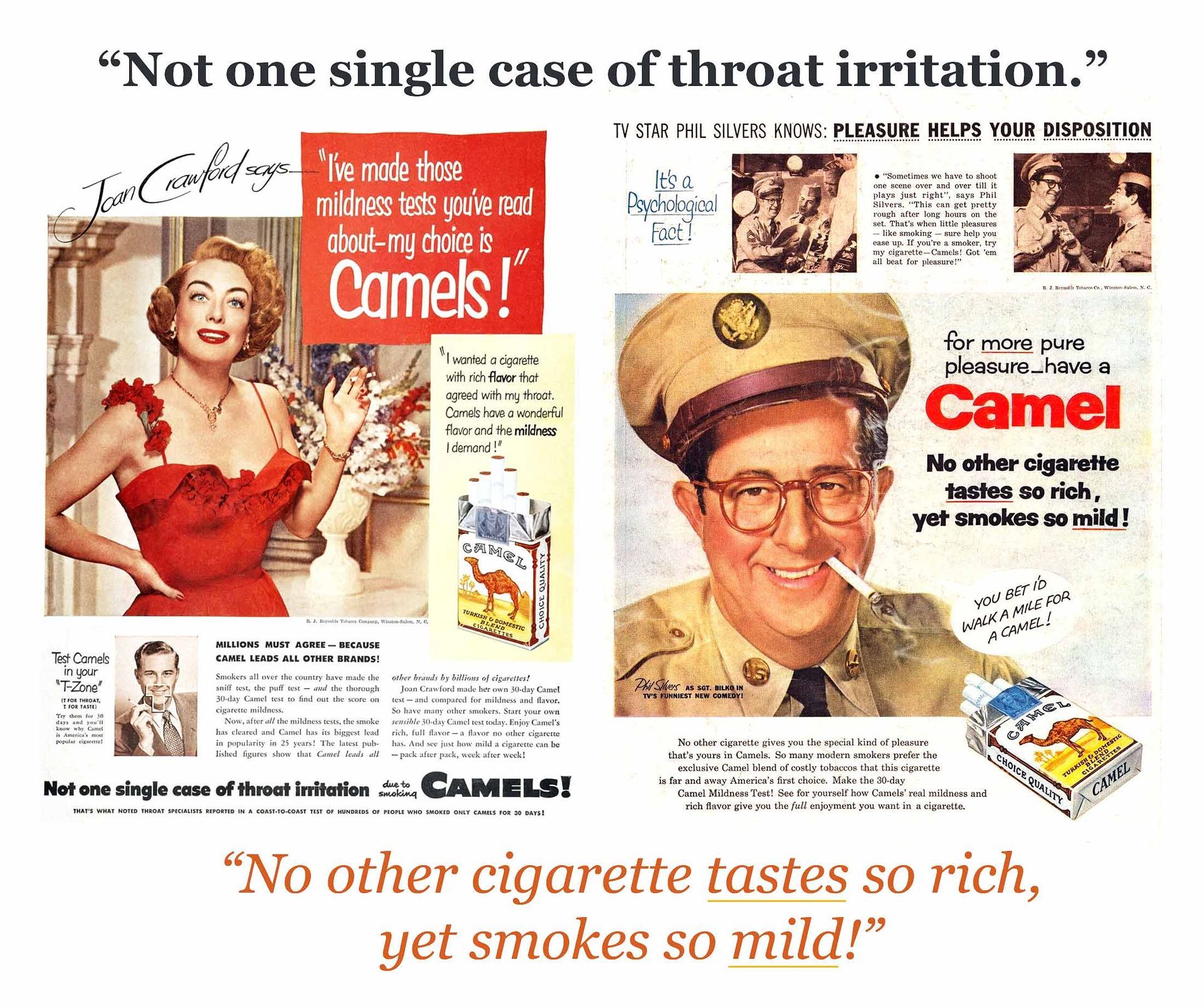
While the short-term effects of COVID-19 can be flu-like, even mild cases can lead to long COVID [Post-Acute Sequelae of COVID-19, or PASC].
Because COVID-19 typically affects breathing and can lead to problems such as pneumonia, many people may think it’s primarily a lung disease.
It’s not that simple, said Dr. Nisha Viswanathan, director of the long COVID program at the David Geffen School of Medicine at the University of California, Los Angeles.
“I would argue that COVID-19 is not a disease of the lungs at all,” she said.
“It seems most likely that it is what we call a vascular and neurologic infection, affecting both nerve endings and our cardiovascular system.”
It’s no surprise that experts say SARS-CoV-2 – the name of the virus that causes COVID-19 – is complex, with many of its pathways just beginning to be understood. But some things are becoming clear.
One of the best reviews of long COVID symptoms appeared last January [2023] in Nature Reviews Microbiology. It detailed the disease’s effects throughout the body, including the pancreas, blood vessels and reproductive system.
“SARS-CoV-2 is excellent at triggering your immune system to go from zero to 100,” said Dr. Lindsay McAlpine, a neurologist who is director of the Yale NeuroCovid Clinic.
That revving of the immune response leads to both a “wide swath of inflammation” and excessive blood clotting.
“Perhaps the viral replication is going on in the lungs and nasopharynx [the area at the top of the throat that connects the nose to the respiratory system]. But the inflammation that the virus triggers is systemic.”
❦ The brain & nervous system
“The virus and the immune response can have several different effects on the brain,” said McAlpine, lead author of a 2021 study looking at ischemic strokes in people with COVID-19.
The exact causes of brain-related issues are not clear, but she said it does not appear that the virus is directly attacking brain tissue.
‘Rather, it seems that the ramped-up immune response leads to clots that could cause brain problems.’
“In addition to the cognitive impairment, we see worsening or new-onset migraines,” she said. “We see new neuropathy in the legs and the arms – numbness, tingling, difficulty walking because of the neuropathy.”
COVID-19 might also be unmasking other neurodegenerative conditions, such as Parkinson’s disease, she said. McAlpine has diagnosed new cases of Alzheimer’s disease in people who, before COVID-19, were functioning fine, then developed symptoms.
❦ The heart & blood vessels
The risk of dangerous clotting – including deep vein thrombosis (clots in large veins) and pulmonary embolisms (clots in the lungs) – is small but stays elevated for up to a year after the infection.
Many factors might be playing into COVID-related heart problems, including microclots – tiny blood clots – or an autoimmune response targeting heart muscle cells.
A recent study in Nature Cardiovascular Research shows the virus may infect coronary arteries, causing plaque build-up to become inflamed and break off, which can lead to a heart attack.
❦ The Gastrointestinal system
“Interestingly, the GI system’s mechanism may be a little different than what impacts the heart,” Viswanathan said. One theory suggests that the virus finds a [‘safe’] hiding place while the rest of the body fights it off.
“And we have found now in multiple studies that COVID can remain in our GI tract for weeks and months after it has resolved in the rest of the body.”
The exact place where the virus might hide is up for debate. But gastrointestinal symptoms are clear: “People can have nausea, vomiting, diarrhea.”
A large study of veterans published last year [7 Mar 2023] in Nature Communications found people with COVID-19 had a higher risk of gastroesophageal reflux disease, irritable bowel syndrome and other gastrointestinal problems more than 30 days after infection compared to people without COVID-19.
The risk was elevated even among people who had mild cases of the disease.
❦ The Kidneys
Kidney problems were common in a 2023 study published in The Lancet Respiratory Medicine that looked at organ damage after COVID-19 infection.
❦ What to do?
The first step is to be cautious if COVID-19 is surging in your area. Consider wearing a mask in crowded public places.
[If you don’t want repeat reinfections, and their cumulatively higher risk of life-altering or fatal consequences, wear a well-fitting (N95/N99 or FFP2/FFP3) respirator in all public spaces, particularly in the highest-risk settings of healthcare, education and transport.]
“A lot of people have COVID now, and it may take a while for them to test positive.
The second thing is get vaccinated.”
The [USA’s] Centers for Disease Control and Prevention recommends everyone ages 5 and older get the updated COVID-19 vaccine to avoid getting seriously ill from the virus.*
* [Pre-2025 Trump election in the USA. Pre-2024 Summer / Autumn / Winter cancellation of SARS-CoV-2 vaccines for those aged 50-plus in the UK.]
“The third thing is controlling your cardiovascular risk factors,” she said. That means getting high blood pressure, diabetes or other chronic medical conditions under control.
McAlpine added that if you have COVID-19 symptoms, stay away from other people to avoid putting them at risk.
“And if you could avoid an illness like COVID or the flu – why wouldn’t you?”’
❂
📖 (16 Jan 2024 ~ American Heart Association) Beyond breathing: How COVID-19 affects your heart, brain and other organs ➤
© 2024
Michael Merschel
/
American Heart Association.
‘Beyond breathing: How COVID-19 affects your heart, brain and other organs.’
© 2024 Michael Merschel / American Heart Association.
❦ Further reading on the heart
(25 Feb 2025 ~ C19.Life) ‘The beating heart... 70 studies and articles on SARS-CoV-2 and the cardiovascular system (2020–2024) ➲’.
❂
‘Results from this study indicated a statistically significant increased risk for a range of cardiovascular conditions as well as mortality.
While these risks were heightened for individuals who experienced a more severe acute episode of COVID-19 (ie. requiring hospitalization), it is essential to note that most individuals (72.5%) in the cohort did not experience hospitalization during the acute phase.
Many of these conditions will have lasting effects on quality of life.’ ➤
© 2023 DeVries et al / JAMA Network.
❂
More... Cardiovascular system