📖 Post-exertional malaise among people with long COVID compared to myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS)
‘Low and medium physical and cognitive exertion triggered PEM for both Long COVID respondents and ME/CFS patients.
Long COVID respondents indicated that high physical and cognitive exertion, stress, food or chemical sensitivities, temperature extremes, insufficient sleep, and illness were significantly more likely to trigger PEM than reported by ME/CFS patients.’
📖 (7 Mar 2023 ~ WORK: A Journal of Prevention, Assessment & Rehabilitation) Post-exertional malaise among people with long COVID compared to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
© 2023 Vernon et al / WORK.
❦ Study ~ ‘Post-exertional malaise among people with long COVID compared to myalgic encephalomyelitis / chronic fatigue syndrome (ME/CFS)’
By Vernon et al / WORK: A Journal of Prevention, Assessment & Rehabilitation (7 Mar 2023) [Abridged]
❦ ‘Little attention and resources have been dedicated to the chronic consequences of acute infection even though examples of post-infectious sequelae from epidemics around the world are common.
✺ The ongoing Chikungunya virus epidemic has caused more than 10 million cases of chronic, debilitating rheumatic disease.
✺ Ebola virus disease survivors suffer from fatigue, insomnia, and depression.
✺ Post-West Nile virus sequelae include muscle weakness, memory loss, and difficulties with activities of daily living.
✺✺ The long-term effects from the 2003 severe acute respiratory syndrome (SARS) outbreak included chronic fatigue, pain, weakness, depression, and sleep disturbance symptoms.
✺ People that recover from infectious mononucleosis, epidemic polyarthritis and Q fever experience disabling chronic fatigue, pain and ‘brain fog’, with 11% of people meeting criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) 12 months after acute illness.
❂
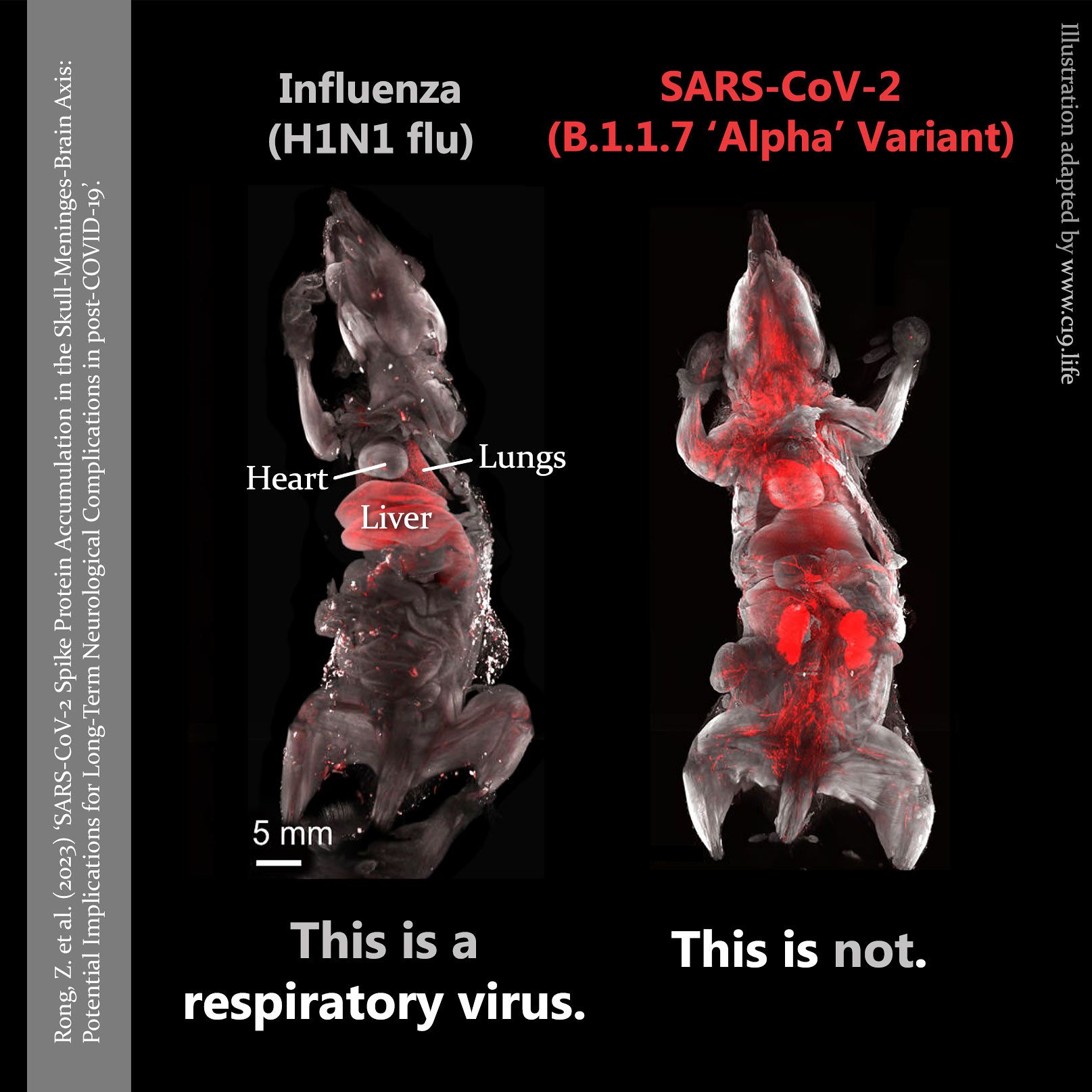
It is estimated that 10-30% of people remain ill for many months after acute COVID-19 with an illness similar to ME/CFS.
Long COVID describes a condition with symptoms that linger for months to years following acute COVID-19.
For ME/CFS patients, physical and cognitive exertion that was easily tolerated prior to illness now triggers a worsening of disease symptoms.
Low and medium physical and cognitive exertion triggered PEM for both Long COVID respondents and ME/CFS patients.
Long COVID respondents indicated that high physical and cognitive exertion, stress, food or chemical sensitivities, temperature extremes, insufficient sleep and illness were significantly more likely to trigger PEM than reported by ME/CFS patients.
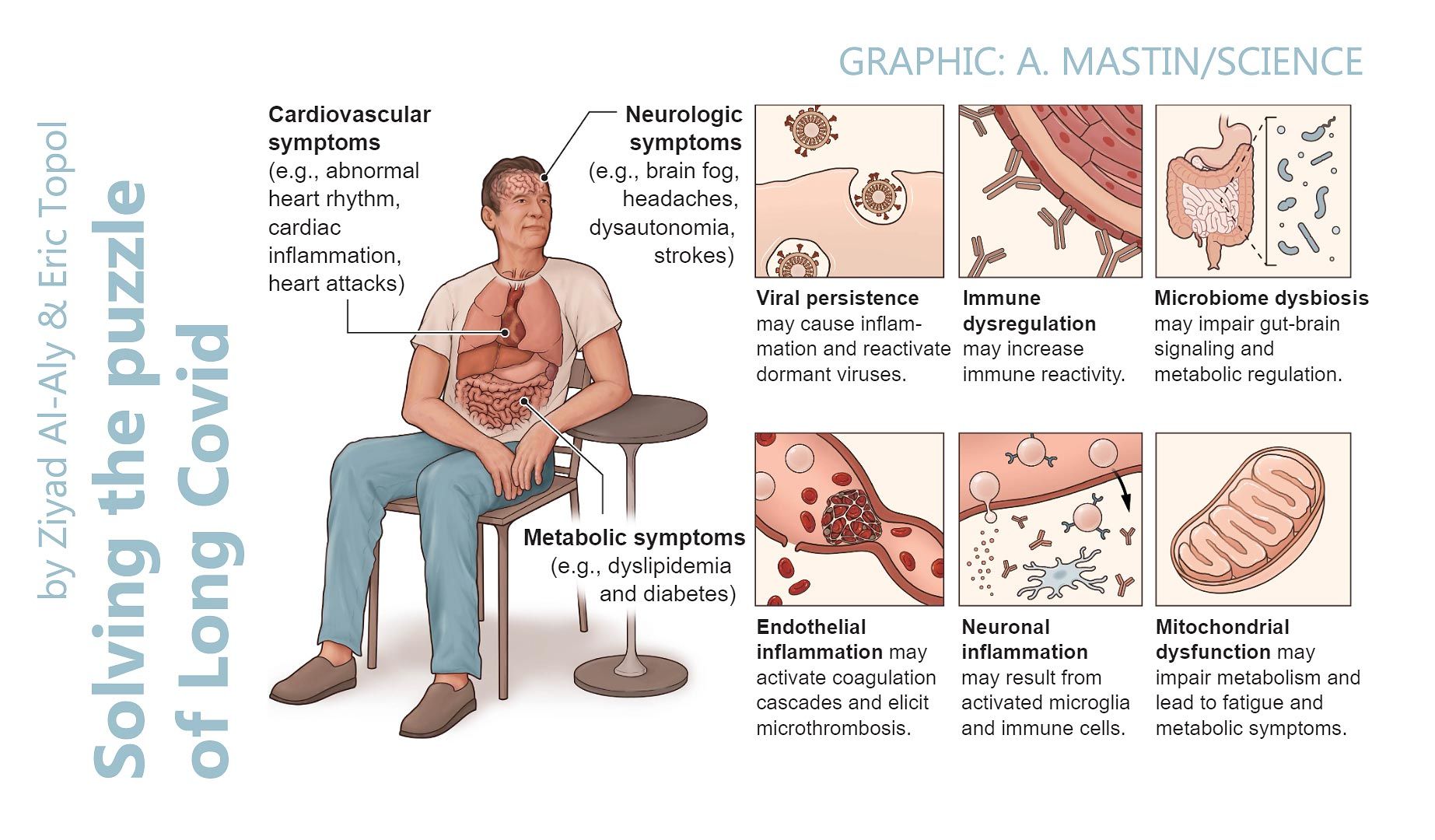
Fatigue, musculoskeletal/pain, orthostatic intolerance, and neurologic symptoms are a common PEM symptom constellation experienced by most ME/CFS patients.
Long COVID respondents reported significantly more sleepiness, respiratory issues, depression and anxiety, irregular body temperature and excessive thirst than ME/CFS patients.
‘Depression and anxiety, both associated with neuroinflammation, were the most frequent neuropsychiatric sequelae of COVID-19.’
There is increasing evidence for the role of neuroinflammation in Long COVID because of SARS-CoV-2 neurotropism and neuroimmune pathophysiology.
‘Similarities between Long COVID and ME/CFS included low and medium physical and cognitive exertion to trigger PEM, symptoms of fatigue, pain, immune reaction, orthostatic intolerance, neurologic and gastrointestinal symptoms during PEM, rest-to-recover from PEM, and pacing to prevent PEM.’
In conclusion, there were significant differences in PEM experienced by people with Long COVID compared to patients with ME/CFS.’
❂
📖 (7 Mar 2023 ~ WORK: A Journal of Prevention, Assessment & Rehabilitation) Post-exertional malaise among people with long COVID compared to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) ➤.
© 2023 Vernon et al / WORK.
More... Post-Exertional Malaise (PEM)


More... PASC (PCS / ‘Long Covid’)