📖 NHS Estates Technical Bulletin ~ Application of HEPA filter devices for air cleaning in healthcare spaces: guidance and standards
‘This document aims to serve as interim guidance and a regulatory reference point for the design and correctly-engineered deployment of HEPA filter devices in real-world settings with regard to effectivity and safety.
It focuses on HEPA filter-based devices which can be positioned locally within a room.
The emergence of SARS-CoV-2 as a highly contagious virus has demanded new and innovative solutions to safeguard patients, staff, and visitors.’
✾
📖 (2 Oct 2023 ~ NHS England) NHS Estates Technical Bulletin (NETB 2023/01A): application of HEPA filter devices for air cleaning in healthcare spaces: guidance and standards.
➲ Date published by NHS England: 9 May 2023.
➲ Date last updated: 2 Oct 2023.
Accessed: 4 Dec 2023.
© 2023 NHS England.
NHS Estates Technical Bulletins (NETBs) enable updated guidance to be passed to local systems, ensuring we maintain our focus on patient safety.
NETBs contain technical guidance and standards which systems and organisations are required to consider and implement, where applicable.
Boards
are
responsible
for their
assessment and application
to their organisations.
NHS Estates Technical Bulletin (NETB 2023/01A) ~ Application of HEPA filter devices for air cleaning in healthcare spaces: guidance and standards
❦ Applicability
This NETB applies to all healthcare spaces with ventilation requirements.
❦ Objective
To provide additional technical guidance and standards on the use of HEPA filter devices for air-cleaning in healthcare spaces.
❦ Executive summary
Ventilation* is an important line of defence for infection control in the healthcare environment.
Its design and operation are described in Health Technical Memorandum (HTM-03-01).
The current focus on ventilation has highlighted areas of high risk due to poorly performing and inadequate ventilation in hospitals and other healthcare settings.
This may be due to change of room use, age, condition of air-handling plant, lack of maintenance, challenges with effective use of natural ventilation or other.
It is therefore important to bring these facilities up to the minimum specification of current standards, particularly recognising the challenges of COVID-19 and other infections.
Local HEPA filter-based air cleaners (also know as ‘air scrubbers’ [and ‘air-cleaning units’ (ACUs) or ‘air purifiers’]) are one option for improving and supplementing ventilation.
The installation of a High Efficiency Particulate Air (HEPA) filter air-cleaner can reduce the risk of airborne transmission.
This guidance has been written as an interim specification to set the basic standard required for HEPA filter devices to be utilised in healthcare and patient-related settings.
This edition is primarily aimed at portable and semi-fixed (wall-mounted) devices.
Devices relying on
ultraviolet light (UVC) are the subject of a separate guidance document:
Application of ultraviolet (UVC) devices for air cleaning in occupied healthcare spaces ➲.
nb. * Ventilation is the process by which ‘fresh’ air (normally outdoor air) is intentionally provided to a space and stale air is removed.
This may be achieved by mechanical systems using ducts and fans, or natural ventilation most commonly provided through opening windows.
The local redistribution of air may also be construed as ventilation.
✾
1. Introduction
Ventilation is an important feature in the control of airborne infection.
However, the emergence of SARS-CoV-2 as a highly contagious virus has demanded new and innovative solutions to safeguard patients, staff, and visitors.
Health Technical Memorandum 03-01 Specialised Ventilation for Healthcare Premises (HTM-03-01) is a robust standard for ventilation of higher risk clinical spaces based on high air-change rates using outdoor air to continually flush indoor spaces.
‘The COVID-19 pandemic has shown that greater attention must be paid to the improvement and maintenance of ventilation in healthcare settings.’
The COVID-19 pandemic has shown that greater attention must be paid to the improvement and maintenance of ventilation in healthcare settings.
The focus on ventilation has also highlighted areas of high risk due to poorly performing and inadequate ventilation, particularly in older hospitals and other healthcare settings such as primary care and dental suites, which increase risks of nosocomial infections.
In cases where current ventilation does not meet HTM-03-01 standards, this may be due to age, condition of air handling plant, lack of maintenance or other design or operational issues.
In the case of naturally ventilated spaces, there is a reliance on staff or patients opening windows. Weather conditions, external noise and air pollution, and restricted window openings for safety affect the ability to open windows and means that ventilation in some settings can fall below recommended rates.
‘Local HEPA filter air cleaners are one option for improving and supplementing ventilation.’
Local HEPA filter air cleaners are one option for improving and supplementing ventilation.
The correct installation and operation of a HEPA filter air cleaner can reduce the risk of airborne transmission.
Healthcare trusts are under pressure to improve ventilation and in the meantime are considering options including filter-based air cleaning.
This standard will assist trusts in selecting and implementing good quality, reliable equipment.
‘There is substantial evidence from laboratory studies and real-world settings that filtration is an effective technology for reducing airborne pathogens within room air and HVAC systems.’
There is substantial evidence from laboratory studies and real-world settings that filtration is an effective technology for reducing airborne pathogens within room air and HVAC systems.
A number of research studies have been carried out which indicate that measured levels of micro-organisms in air are greatly reduced by air filters [R1-R5, R7].
There is also evidence which directly associates use of filter-based air cleaners with reductions in infection rates of environmentally-derived aspergillus [R8].
The potential of air scrubbers employing UVC or HEPA technology to mitigate SAR-CoV-2 risks is the subject of a rapid review (September 2022) [R.9].
Filter-based air cleaners also remove other particulate matter and so can also reduce exposure to other air pollutants.
However, air cleaners should not be used as a reason to reduce ventilation and care must be taken to ensure sufficient fresh air changes are provided for the dilution of medical gases and noxious odours, and the maintenance of appropriate oxygen and carbon dioxide levels to satisfy the Building Regulations Part F.
This document aims to serve as interim guidance and regulatory reference point for the design and correctly engineered deployment of HEPA filter devices in real-world settings with regard to effectivity and safety.
It focuses on HEPA filter-based devices which can be positioned locally within a room; the document does not cover HEPA filters used within HVAC ducts.
Local filter-based devices require fan-assisted circulation to introduce the room air into the device, pass it through the filters and then to reintroduce the processed air into the room.
An important consideration regards the flow of the air which is induced, processed and distributed by the device external to the device itself.
The
design
and
placement
of the device should
promote efficient air distribution
in the room space and avoid short-circuiting of air circulation relative to furniture, obstructions, and occupancy.
✾
2. HEPA filter technology
HEPA filters comprise a porous structure of fibres or membrane which remove particles carried in an air stream.
The mechanism by which particles are removed depends on the size of the particle.
Larger particles are removed by impaction onto the filter while smaller particles <1 μm are removed through interception and diffusion.
Interception occurs where the particle makes physical contact with the media fibres because particle inertia is not strong enough to enable the particle movement to continue.
Diffusion is where random motion (Brownian motion) of the particle enables it to contact the media.
These effects are enhanced by the electrostatic charges present on filters.
2.1 ~ Selection of filters
Filter efficiency defines the fraction of particles removed and varies by size of particle.
The most difficult size of particles to remove, known as the most penetrating particle size (MPPS), for the majority of filters is around 0.3 μm; particles larger or smaller than this size are captured more effectively.
For healthcare applications it is recommended that devices should contain filters classified as High Efficiency Particulate Air Filters (HEPA) under BS EN 1822-1 or ISO 29463-1.
HEPA filters have a filter efficiency of at least 99.95% (H13 filter) or 99.995% (H14 filter) for the MPPS, however the performance in situ is sometimes lower depending on the filter and device design and the air flow rate (section 5.1).
Micro-organisms range in size from around 0.1 μm for the smallest viruses to several μm in diameter for larger bacteria and fungi.
Some fungi and bacteria may be dispersed independent of other material, however, many pathogens will be released on or within another material and therefore the size of the particle that needs to be captured is larger than the pathogen itself.
For example, respiratory and gastroenterology viruses will be released within liquid media that contains proteins, salts, surfactants, etc and evaporates to form particles that are larger than the virus itself.
Similarly, many skin-associated bacteria are released on skin squame which are larger than the bacteria.
Some filter-based air cleaning devices contain lower grades of filter.
These devices may be appropriate in non-clinical areas, but as the filters have a lower performance for particles relevant to the size of airborne pathogens they are not recommended in settings with vulnerable patients.
It is common for HEPA filter-based devices to incorporate a coarse grade of filter (typically ISO ePM10 >50% under ISO 16890-1) to act as a dust filter.
Some also include a carbon filter to manage odours and volatile organic compounds.
Some devices contain several separate filters, while others incorporate the different-stage filters into a single-cartridge-type unit.
2.2 ~ Inclusion of other technologies
Devices which include germicidal ultraviolet (UVC) light alongside HEPA filters are likely to be effective [R4].
Where these devices are considered, this standard takes precedence in terms of clean air performance if the UVC lamp is located after the HEPA filter (i.e. the HEPA filter is the primary device for microbial removal).
However, all the safety requirements pertaining to the UVC within that standard should also be complied with.
[Note:] Devices which incorporate ionisation, photocatalytic oxidation, electrostatic precipitation or other similar technologies alongside filters are not currently recommended for healthcare use unless there is clear evidence for both effectiveness and safety.
These devices can sometimes introduce, or create through secondary reactions, chemical by-products into a room which may themselves have an adverse health effect [R4, R11].
The independent research evidence that these products are any more effective at safely reducing microbial loads in air is still emerging.
✾
3. Applications and sizing
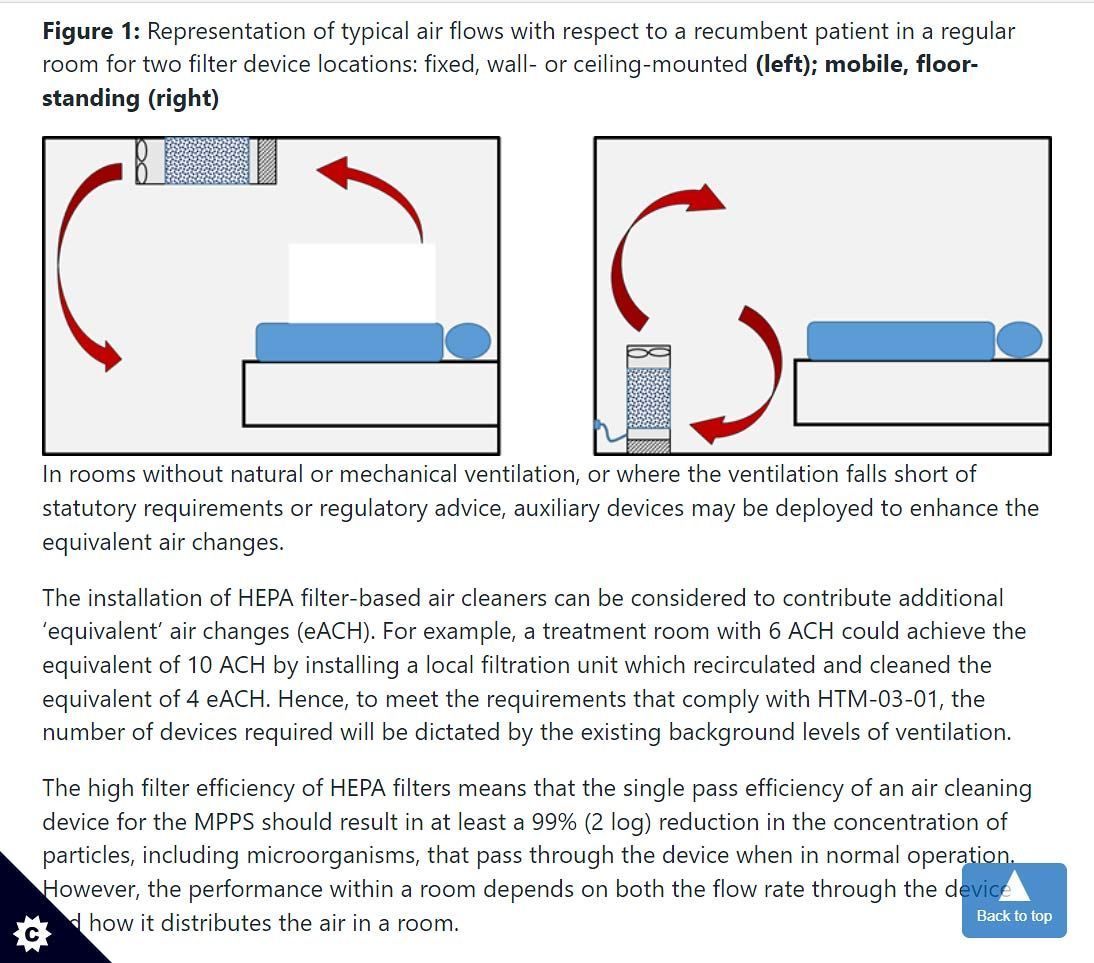
‘Stand-alone, floor-mounted devices can be positioned at any suitable location in a room.’
Stand-alone, floor-mounted devices can be positioned at any suitable location in a room.
These devices are plugged into a standard electrical socket so do not require any installation, although location is important as detailed in sections 8.2 and 8.3.
Fixed devices are semi-permanently mounted to a wall or ceiling.
These devices will normally be permanently wired into the room electrical systems rather than plugged into a wall socket. Some manufacturers offer local systems that can be interfaced with the ventilation system and are able to offer pressure differential control in a room.
‘In rooms without natural or mechanical ventilation, or where the ventilation falls short of statutory requirements or regulatory advice, auxiliary devices may be deployed to enhance the equivalent air changes.’
In rooms without natural or mechanical ventilation, or where the ventilation falls short of statutory requirements or regulatory advice, auxiliary devices may be deployed to enhance the equivalent air changes.
The installation of HEPA filter-based air cleaners can be considered to contribute additional ‘equivalent’ air changes (eACH).
For example, a treatment room with 6 ACH could achieve the equivalent of 10 ACH by installing a local filtration unit which recirculated and cleaned the equivalent of 4 eACH.
Hence, to meet the requirements that comply with HTM-03-01, the number of devices required will be dictated by the existing background levels of ventilation.
The high filter efficiency of HEPA filters means that the single pass efficiency of an air cleaning device for the MPPS should result in at least a 99% (2 log) reduction in the concentration of particles, including microorganisms, that pass through the device when in normal operation.
However, the performance within a room depends on both the flow rate through the device and how it distributes the air in a room.
The performance of filter-based devices is described by some manufacturers in terms of a Clean Air Delivery Rate (CADR) which is usually expressed in metres cubed per hour (m3h-1) (some devices quote the CADR in cubic feet per minute, cfm).
Where a CADR is given it should be derived from measurements of how well the device removes a defined size of particles in a test room environment; CADR is usually measured using particles rather than microorganisms.
CADR is a function of the airflow rate through the device, the quality of the filter and the way the device distributes air in the test room.
Other manufacturers adopt different metrics such as the time to reduce particle concentrations in a room by a specific percentage.
The CADR or other metrics can be used, with care, for design purposes as they express how the device will perform in a standardised test room.
However, it is important to note that the actual performance will depend on the particular location and operation of the device, including the room size, layout, background ventilation, device design and maintenance (section 8).
It is not recommended to use an air cleaning device with a lower grade of filter even if the quoted CADR is high, as the device may be less effective against the smallest pathogen-carrying particles.
The CADR used for design purposes should be the rate applicable to the device setting at which the device is most likely to be operated and where the noise level is during operation is at a level of ≤50 dB measured at 3 m (dB3m) (section 5.3).
✾
➲
For the
full NHS Estates Technical Bulletin
document, please refer to the
link
at the
bottom of this page.
✾
❦ Bibliography
Laboratory chamber studies demonstrating effectiveness of HEPA filter devices against particles and microorganisms
- [R1] Miller-Leiden S, Lohascio C, Nazaroff WW, Macher JM (1996) Effectiveness of in-room air filtration and dilution ventilation for tuberculosis infection control. Journal of the Air & Waste Management Association 46: 869–882. doi:10.1080/10473289.1996.10467523
- [R2] Offermann FJ. et al (1985) Control of respirable particles in indoor air with portable air cleaners. Atmospheric Environment 19: 1761–1771. doi:10.1016/0004-6981(85)90003-4
- [R3] Ueki H, Ujie M, Komori Y, Kato T, Imai M, Kawaoka Y (2022) Effectiveness of HEPA filters at removing infectious SARS-CoV-2 from the air. mSphere 7(4):e0008622. doi:10.1128/msphere.00086-22.
- [R4] Beswick A, Brookes J, Rosa I et al. 2022. Room based assessment of mobile air cleaning devices using a bioaerosol challenge. Applied Biosafety Journal. Published online Dec 2022. doi:10.1089/apb.2022.0028
- [R5] Lindsley WG et al (2021) Efficacy of portable air cleaners and masking for reducing indoor exposure to simulated exhaled SARS-CoV-2 Aerosols — United States, 2021. Morbidity and Mortality Weekly Report (MMWR) 70: 972—976. doi:10.15585/mmwr.mm7027e1
Testing approach for Clean Air Delivery Rate (CADR)
- [R6] Foarde KK, Myers EA, Hanley JT, Ensor DS, Roessler PF (1999) Methodology to perform clean air delivery rate type determinations with microbiological aerosols. Aerosol Science and Technology 30: 235–245. doi:10.1080/713834074
Application of HEPA devices in healthcare setttings
- [R7] Conway Morris A, Sharrocks K, Bousfield R, et al, The Removal of Airborne Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Other Microbial Bioaerosols by Air Filtration on Coronavirus Disease 2019 (COVID-19) Surge Units. Clinical Infectious Diseases, Volume 75, Issue 1, 1 July 2022, Pages e97–e101, doi:10.1093/cid/ciab933
- [R8] Abdul Salam ZH, Karlin RB, Ling ML, Yang KS. The impact of portable high-efficiency particulate air filters on the incidence of invasive aspergillosis in a large acute tertiary-care hospital. American Journal of Infection Control. 2010 May;38(4):e1-7. doi:10.1016/j.ajic.2009.09.014.
- [R9] Bowles C, et al. A rapid review of supplementary air filtration systems in health service settings. September 2022. doi:10.1101/2022.10.25.22281493 medrxiv preprint.
Wider reading on air-cleaning applications
- [R10] Medical Advisory Secretariat. Air cleaning technologies: an evidence-based analysis. Ontario health technology assessment series vol. 5 (2005) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3382390/
- [R11] SAGE-EMG:
Potential application of air cleaning devices and personal decontamination to manage transmission of COVID-19, 4 November 2020.
https://www.gov.uk/government/publications/emg-potential-application-of-air-cleaning-devices-and-personal-decontamination-to-manage-transmission-of-covid-19-4-november-2020
✾
📖 (2 Oct 2023 ~ NHS England) NHS Estates Technical Bulletin (NETB 2023/01A): application of HEPA filter devices for air cleaning in healthcare spaces: guidance and standards ➤
➲ Date published by NHS England: 9 May 2023.
➲ Date last updated: 2 Oct 2023.
Accessed: 4 Dec 2023.
© 2023 NHS England.