by Ryan Hisner
•
17 February 2022
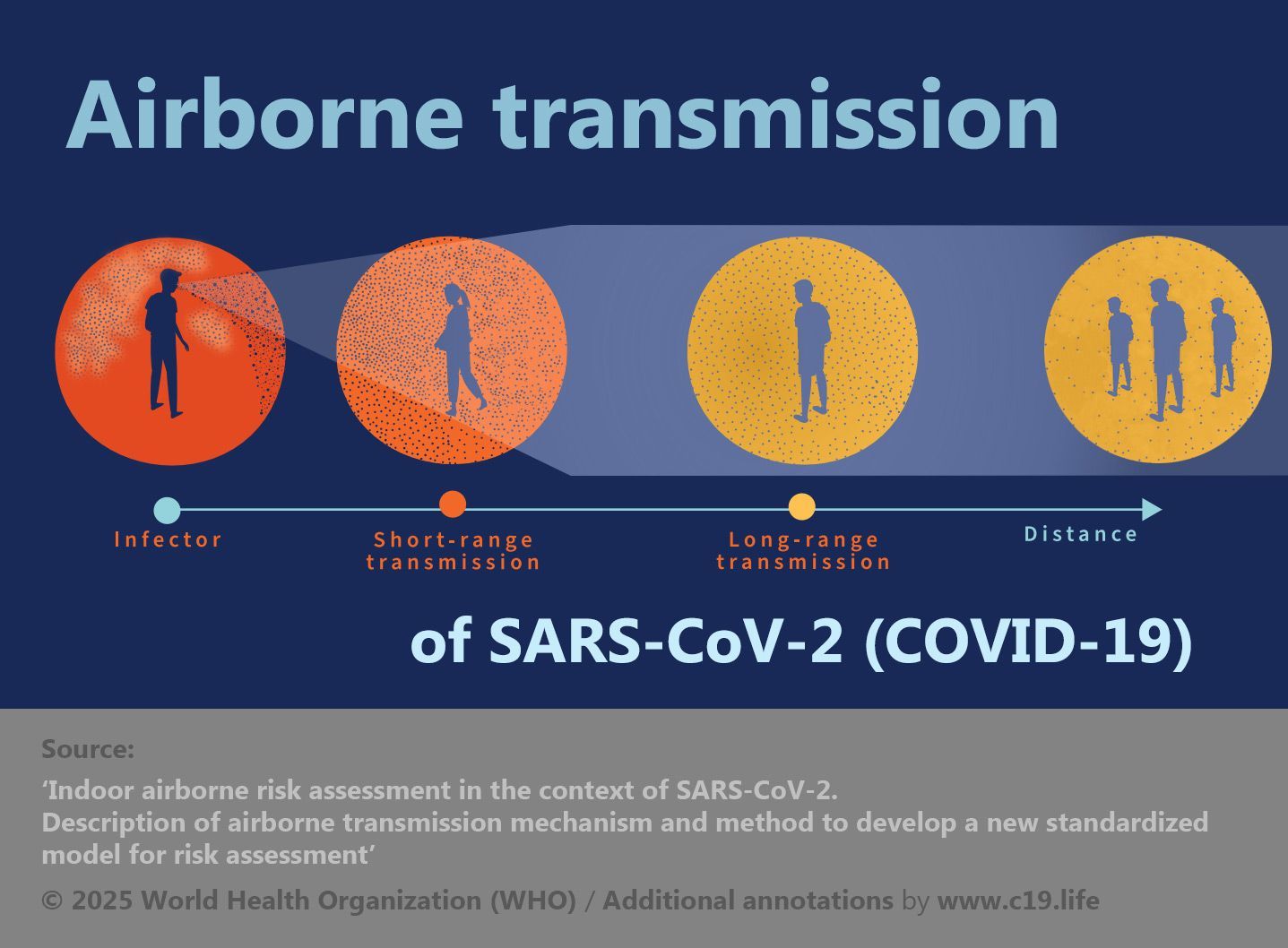
Ryan Hisner pulls apart the real-life Animal Farm theatre playing out between Man, Pig and The Economy in his 2022 essay on swine, clean air, and bringing home the bacon. ✾ ❦ “What should be a higher priority for society: preventing pigs from becoming sick, or preventing human illness? Personally, I place a higher value on preventing human illness. I think most would agree. Why, then, are pig barns far better ventilated than schools? An airborne virus has killed 900,000 Americans, and has left countless others suffering from Long Covid along with its chronic, and perhaps permanent, mental and physical afflictions. We know that ventilation and the filtration of indoor air prevents illness. The manifold benefits of improved ventilation are well-documented and uncontroversial. Professor Don Milton has been publishing studies for over twenty years showing that improved ventilation reduces respiratory illnesses and absences, though his findings were largely ignored. Yet we’ve done almost nothing to improve air filtration and ventilation in schools, workplaces, restaurants, and other buildings. The USA’s CDC (Centers for Disease Control and Prevention) gives lip service to ventilation – but has issued no minimum ventilation requirements, and offers no specific guidance. 📖 (26 Feb 2021 ~ CNN Health) CDC must encourage better ventilation to stop coronavirus spread in schools, experts say ➤ On the other hand, great cost and effort is put into ventilating and filtering the air in pig barns in order to prevent disease outbreaks. Let’s compare the ventilation and air-filtration of pig barns with buildings inhabited by human beings. First, note that airborne spread of Porcine Reproductive and Respiratory Syndrome (PRRS) was readily accepted based on circumstantial evidence and lab studies. French farms even installed HEPA filtration systems in pig barns, despite “no hard data to support” their use. Contrast this with the stubborn, year-long denial of airborne Covid spread by the WHO and CDC, despite abundant evidence. The precautionary principle is obeyed when pigs’ health is at stake, but not when human health is at risk. Incredibly, droplet dogma still reigns supreme in some places. Many are still fighting against appallingly ignorant public officials and nonsensical guidelines in Australia. [Insert ubiquitous poster from your hospital, doctor’s surgery, pharmacy, bowling alley or supermarket extolling the virtues of hand-washing and hand-sanitiser in a pandemic essentially driven by aerosol transmission .] Some officials haven’t gotten the memo yet: Covid is airborne . Many careful, controlled studies of ventilation and air-filtration in livestock facilities have been carried out, and the cumulative evidence compiled leaves little doubt of their effectiveness at preventing disease in farm animals. One of many examples: 📖 (July 2006 ~ Canadian Journal of Veterinary Research) Further evaluation of alternative air-filtration systems for reducing the transmission of Porcine reproductive and respiratory syndrome virus by aerosol ➤ In contrast, before Covid, research on ventilation, air-filtration and disease in human dwellings was pretty sparse. Linsey Marr, Don Milton, Julian Tang, Yuguo Li and others were lone voices in the wilderness, shouting into a void, and ignored by the CDC and the WHO. For buildings that humans inhabit, enforced minimum ventilation requirements are almost non-existent. The HVAC* in a school or nursing home can be completely non-functional, creating a superspreader environment, and with no legal consequences. * HVAC = Heating, Ventilation, and Air Conditioning. This is not hypothetical. Here is one documented instance in which all 226 residents in a Canadian nursing home contracted Covid, resulting in over 70 deaths. 📖 (14 May 2020 ~ CBC News) Investigators look into catastrophic outbreak that infected all residents of TMR seniors' home, killing 70 ➤ The cause? A non-functioning ventilation system. And this was a less transmissible, pre-Alpha SARS-CoV-2 variant. 📖 (15 May 2020 ~ Radio Canada) Un CHSLD infecté à 100%, avec un système de ventilation en panne, préoccupe Québec ➤ The same private company owned another nursing home in which 96% of residents and 116 employees caught Covid, leading to the death of 66 residents. I think we can surmise that the ventilation in this facility was also very poor. Why were the ventilation systems in these nursing homes not audited? Because such auditing is simply not done – not in nursing homes, schools, workplaces or restaurants. Ventilation and air-filtration recommendations exist, but not enforced standards. They’re essentially voluntary. What about pig barns? While there are no legal requirements, the ventilation and air-filtration systems at these facilities are assiduously checked every day by a worker whose sole duty is to inspect and maintain the ventilation equipment. 📖 (12 Nov 2016 ~ National Hog Farmer) Hog barn filtration system audits imperative to disease control ➤ No aspect of the system is left unchecked. “Look for any gaps or openings that would allow dirty air in... Make sure chutes collapse properly, creating a good seal.” “Cracked fan housings or a broken shroud” are checked for, and “weep holes plugged with a rubber stopper...” But daily inspection is only the start. In addition, at least once a month, a system filtration technician (SFT) audits the ventilation system, coaching the on-site manager. Another monthly audit is performed by the herd veterinarian, who guides the SFT. In contrast, human dwellings (such as nursing homes) are virtually never audited, even during a pandemic. It apparently requires a court order for such an audit to occur. Are HVAC systems in human-occupied buildings well maintained? HVAC expert Jeffrey Siegel: “The best HVAC in the world performs poorly when it’s not well maintained, and the usual standard is ‘not well maintained’.” The same article* describes an HVAC unit installed upside-down in a large store, making it impossible to change the filter, meaning that “... the air inside the store would be that much crummier”. It was like “a thousand other HVAC mistakes” Siegel has seen: “... dampers supposed to admit outside air into a building rusted open or shut, badly-installed filters letting air pass around their edges, forced-air fans running 18% of the time. In theory, HVAC heats and air-conditions. In practice, it doesn’t always ventilate... or filter.” * 📖 (9 Nov 2020 ~ Wired) The Next Covid Dilemma: How to Make Buildings Breathe Better ➤ What sort of air filters are used for pig barns? First, a mesh net catches larger objects in the air, such as feathers. Then the air goes through a MERV 8 ‘pre-filter’. This pre-filter is of a higher grade than the filters used in many schools, which are MERV 7. After passing through the MERV 8 pre-filter, air entering pig barns is filtered by MERV 15 air filters – similar to the filters used in hospitals. Very few schools, workplaces, nursing homes or restaurants use anything above MERV 11. MERV 15 is unheard of. Does such high-quality ventilation and filtration of pig barns reduce disease outbreaks? Of course it does, as the extensive literature on livestock-facility ventilation and air-filtration attests. 📖 (May 2012 ~ Viruses) Evaluation of the long-term effect of air filtration on the occurrence of new PRRSV infections in large breeding herds in swine-dense regions ➤ However, there is a potential problem: what if some of the dirty air from the human-occupied office building on a farm were to leak into the pig barn? Perish the thought! To allow pigs to breathe the same filthy air breathed by humans would be unthinkable. Therefore, pig farms are designed so that none of the filthy air from the farm’s human office is allowed to contaminate the pristine, highly-filtered air of the pig barn. (“If there is dirty air in the office, it will stay in the office.”) The notion of providing pig-quality air to the office is considered so absurd that it doesn’t merit consideration. After all, if the health of the workers on a farm is improved, this doesn’t affect profits. A sick pig, on the other hand, hurts the bottom line. Priorities... One article on the ventilation and air-filtration of pig barns notes a peculiar “side benefit” of improving the pigs’ air: human workers notice the better air, and seem healthier for it. How much healthier? No-one knows, as such trivial topics as worker health are not researched. So why is the air quality in human buildings so poor? Why haven’t greater efforts been made to improve indoor air quality (IAQ), the enormous benefits of which are well-known and uncontroversial? After all, we regulate water and food safety. Why not indoor air? The WHO recommends schools and other buildings have at least 6 air changes per hour (ACH). A typical school HVAC provides less than 1 ACH. IAQ experts recommend CO2 levels be less than 800 ppm (or less than 700 ppm in a pandemic), but CO2 levels regularly reach much higher levels in schools. I’ve occasionally registered levels near 3000 ppm; others report readings higher than 4000 ppm. What about hotels? I stayed in a room at the Disney Caribbean Resort Hotel with my brother. CO2 reached well over 3000 ppm each night. I did a CO2 decay study, and found that the room got 0.11 air changes per hour. Not good. It’s long past time to greatly improve ventilation and air filtration by imposing serious, enforced IAQ standards in nursing homes, schools, workplaces and other public spaces. Many aerosol and IAQ experts have been calling for this for a long time. 📖 (14 May 2021 ~ Science) A paradigm shift to combat indoor respiratory infection ➤ Only recently have their calls gained traction. The vast majority of people would be much better off if IAQ were improved through better ventilation and filtration. We spend the majority of our lives indoors. Proper air filtration and ventilation would enormously improve the air we breathe. When we think of air pollution, we usually think of lung damage. But polluted air damages all organs of the body. With cleaner air, brain function would improve; heart attacks and strokes would fall; illness would be reduced. It works for pigs. It can work for humans, too. Air pollution is possibly the single largest health problem in the world. It causes the loss of more years of life than alcohol and narcotics, unsafe water, HIV, malaria, and war combined. Cleaning the air we breathe is essential. However, the pecuniary interests of the 1% of landlords, real-estate magnates, business owners, and capitalists in general might not be so well-served. Installing better ventilation systems and air filters in human dwellings might put a dent in their investment returns – an unthinkable notion. To sum up. Improving indoor air quality in human dwellings merely improves the health and well-being of humans – a minor consideration – while improving air quality in pig barns improves profits: a sacred objective, and the chief aim of life under capitalism.” ❂ Related : 📖 (10 Aug 2020 ~ The Conversation) How to use ventilation and air filtration to prevent the spread of coronavirus indoors ➤ Related : 📖 (28 Sep 2020 ~ Quartz) What everyone should know about ventilation and preventing Covid-19 ➤ ❂ © 2022 Ryan Hisner . ➲