on air: transmission
“Infection control guidelines are fundamentally flawed: SARS-CoV-2 is airborne.”
Dr. K. Fearnley, NHS (England) (2023)
❦ on biohazard levels
“Infection control guidelines are fundamentally flawed: SARS-CoV-2 is airborne.
It is outrageous that three-and-a-half years into this pandemic, staff and patients are still, knowingly and repeatedly, being exposed to a Level-3 Biohazard – a virus known to cause brain damage and significantly increased risk of life-threatening blood complications even in those recovered.”
Dr. K. Fearnley, NHS (England) (2023)
➲ Biohazard Level 3 ~ SARS-CoV-2 – the virus that causes COVID-19 – is classed as a Biohazard Level 3.
Other BHL-3 examples include Yellow fever, West Nile virus, plague [Yersinia pestis], and the bacteria that causes tuberculosis (TB).
Biohazard Level 3 pathogens can cause serious or potentially lethal disease in humans.
➲ Biohazard Level 2 ~ Agents that can cause severe illness in humans.
BHL-2 examples include HIV, Zika virus, hepatitis A, B and C, Dengue, and Salmonella.
➲ Biohazard Level 4 ~ The highest biohazard level.
Pathogens that pose a high risk of life-threatening disease for which there are no treatments.
BHL-4 examples include the Ebola virus, Marburg virus, and Lassa virus.
❂ BHL or ‘Biohazard Levels’ are also commonly referred to as ‘Biological Safety Levels’ or ‘Biosafety Levels’ (eg. BSL-3 / BSL-4).
❦ on individual risk assessments
“We cannot individually assess the risk of infection from poor indoor air quality [in public spaces].
Just as we cannot individually assess food safety in restaurants, or fire safety in cinemas, or aviation safety on flights.
These are in the control of others, and are regulated for our health and safety.”
Orla Hegarty (2024)
❦ on nosocomial (hospital-acquired or healthcare-associated) infections
“Every single case in which a person with Covid-19 infects another person in a healthcare setting – patient, relative, or hospital staff member – is a significant failure of hospital procedures.
Every single instance.”
Professor Steve Robson MPH MD PhD ~ President, Australian Medical Association (AMA) (2024)
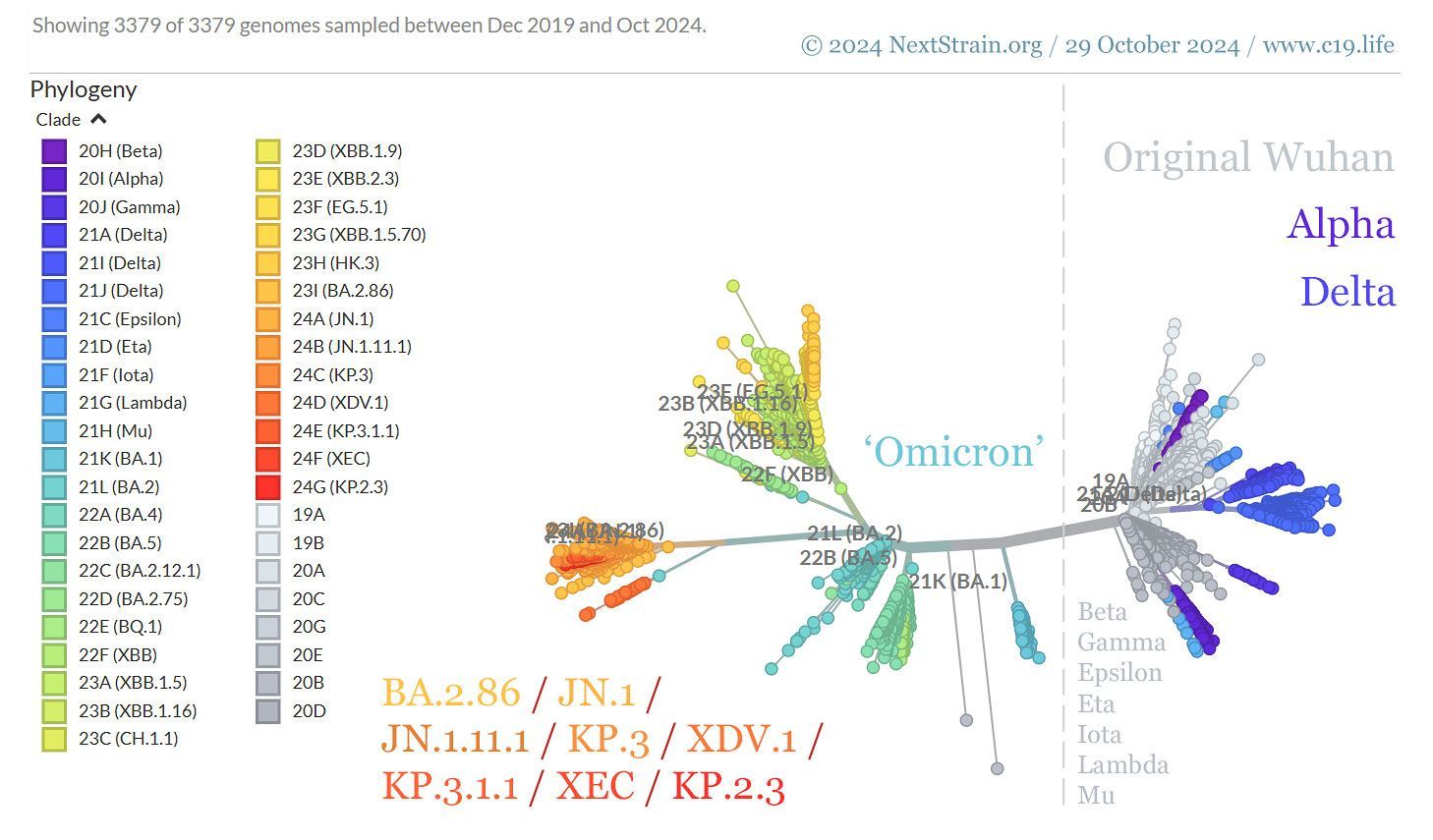
❦ on transmission of SARS-CoV-2
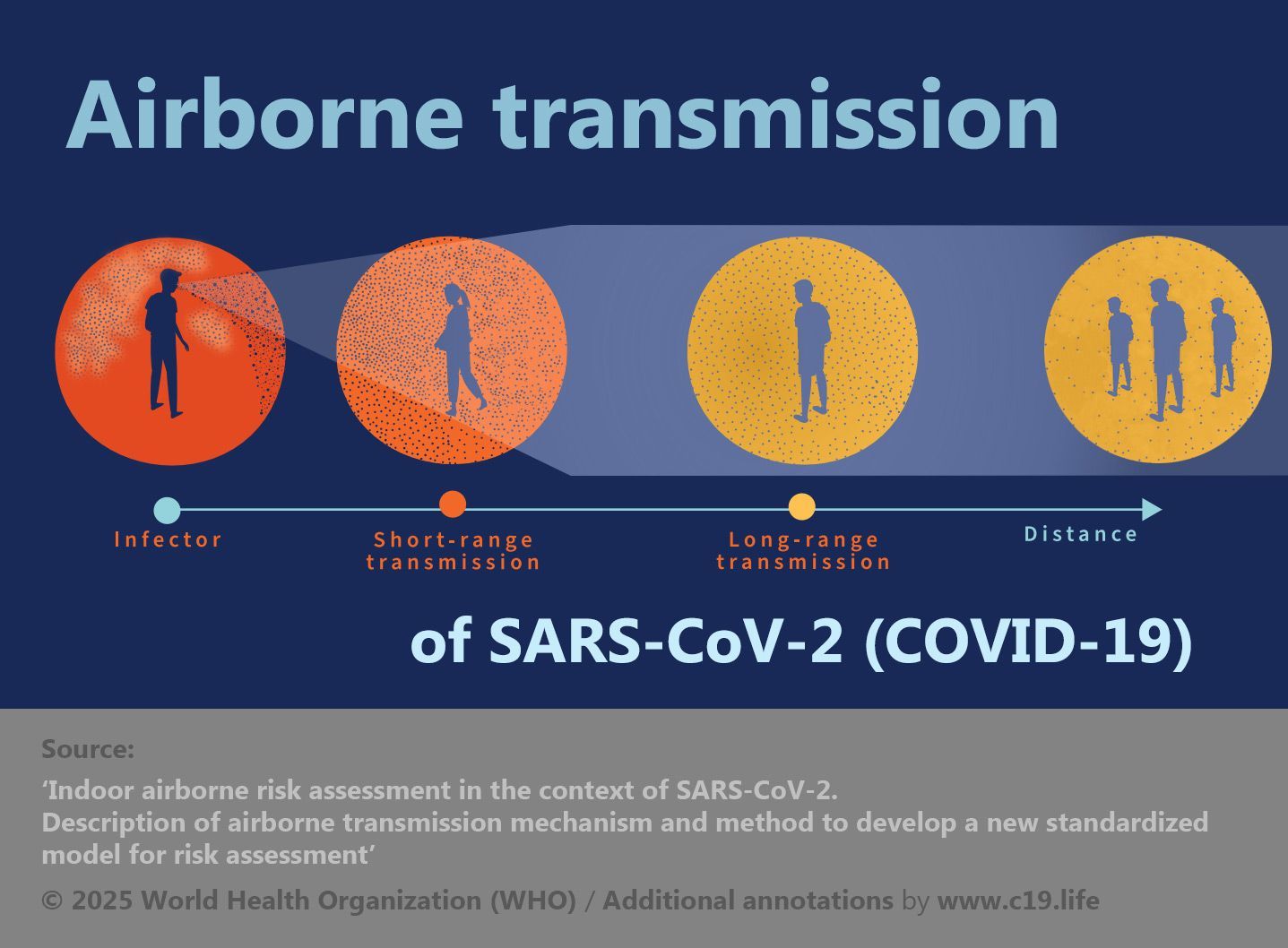
SARS-CoV-2 – the virus that causes Covid-19 – is airborne.
In May 2021, the WHO officially recognised that SARS-CoV-2 is
airborne
via
microscopic aerosols – meaning that the virus is
transmissible through the air at both
long
and
short range.

© 2024 Protect our Province: New Brunswick (PoP NB) ➤
Infections from direct body contact (holding hands) or from fomites (touching infected objects) are low-risk-to-negligible.
The
airborne route, via
aerosol, is acknowledged to be the
dominant
form of transmission.

📖 (13 Jan 2021 ~ Journal of Hospital Infection) Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) ➤
❦ What are ‘aerosols’?
Aerosols are microscopic droplets suspended in the air, and move through a space much like cigarette smoke.

📖 (29 Oct 2020 ~ El País) A room, a bar and a classroom: how the coronavirus is spread through the air ➤
Without air-filtration or ventilation, infectious aerosols remain suspended in the air, becoming increasingly concentrated as time goes by.
© 2020 El País.
While larger droplets are commonly produced by coughing or sneezing, airborne aerosols are produced when a person exhales – including breathing, talking, singing, shouting, coughing or sneezing.

📖 (29 Oct 2020 ~ El País) A room, a bar and a classroom: how the coronavirus is spread through the air ➤
‘Six people get together in a private home, one of whom is infected.
Irrespective of whether safe distances are maintained, if the six people spend four hours* together talking loudly without wearing a face mask in a room with no ventilation, five will become infected.’
* Note: The infectiousness of SARS-CoV-2 has greatly increased since this 2020 scenario: infection times with current 2025 variants can be counted in seconds and minutes than hours.
© 2020 El País.
And while heavier droplets fall to the ground within seconds, infectious aerosols can accumulate and stay airborne for hours in enclosed spaces.

📖 (17 Jun 2020 ~ El País) An analysis of three Covid-19 outbreaks: how they happened and how they can be avoided ➤
© 2020 El País.
Virus-laden aerosols can be present and cause infection long after an infected person has left a room, a shop, a hospital, a GP’s surgery, a pharmacy, a classroom, a bus or a train.

📖 (17 Jun 2020 ~ El País) An analysis of three Covid-19 outbreaks: how they happened and how they can be avoided ➤
© 2020 El País.
‘Buildings play a critical role in minimising, or conversely exacerbating, the spread of airborne infectious diseases.
COVID-19 outbreaks largely occur indoors – and in-room long-range transmission beyond two meters (six feet) has been well-documented in conditions with no masking and low ventilation rates.’
(2021) The Lancet COVID-19 Commission ➤

📖 (29 Oct 2020 ~ El País) A room, a bar and a classroom: how the coronavirus is spread through the air ➤
‘The riskiest scenario [in a school] is a classroom with no ventilation and the teacher – Patient Zero – as the infected person.
If two hours* are spent in the classroom with an infected teacher, without taking any measures to counter the number of aerosols, there is the risk that up to 12 students could become infected.’
* Note: The infectiousness of SARS-CoV-2 has increased greatly since this early 2020 scenario: airborne person-to-person infections at either short- or long-range can be counted in seconds and minutes [2025 variants] than hours.
© 2020 Luis Almodóvar / El País.
Infected asymptomatic people (people who are infectious but not showing symptoms, or up to 60% of cases) may not be aware that they are ejecting virus-laden aerosols into the air that you breathe.

© 2024 Protect our Province: New Brunswick (PoP NB) ➤
Other serious and potentially life-threatening airborne infectious diseases spread by aerosol include Measles, TB (Tuberculosis), Influenza, Highly Pathogenic Avian Influenza (HPAI/H5N1/‘Bird Flu’), Respiratory Syncytial Virus (RSV), Human Rhinovirus (HRV), Pneumonia, Adenovirus, Enterovirus, Severe Acute Respiratory Syndrome Coronavirus (SARS[-CoV-1]), and Middle East Respiratory Syndrome Coronavirus (MERS-CoV).

© 2024 CovidisAirborne.org ➤
❦ human fodder for the ‘frontline’ ~ pt. 1 (2021)
‘Our very serious concerns relate to the risk of aerosol/airborne infection; RCN and BMA members working in all settings are raising concerns that they are not adequately protected.
Our members are concerned that fluid repellent surgical face masks and face coverings, as currently advised in most general healthcare settings, do not protect against smaller more infective aerosols.’
Royal College of Nursing (RCN/UK) / British Medical Association (BMA) (21 Jan 2021) ➲
❦ human fodder for the ‘frontline’ ~ pt. 2 (2023)
‘Figures show that there has been a rise in COVID-19 cases and hospitalisations [in December 2023], and the RCN argues that without proper protections, ill health could continue to rise in nursing staff and impact their ability to deliver safe and effective patient care.
The RCN is urging healthcare employers to assess the risk posed by COVID-19 and put appropriate safeguards in place for patients and staff [regarding the newly-arrived variant JN.1].’
Royal College of Nursing (RCN) ~ (21 Dec 2023) ➲
‘We have heard from a range of multidisciplinary clinicians from across primary and secondary care express concern about the lack of availability of even the most basic protections in many settings when they are treating patients with confirmed or suspected COVID-19.
Ensuring the protection, so far as reasonably practicable, of staff who are vulnerable through exposure to the virus and any staff or patients who are individually susceptible and at risk of serious illness if they catch COVID-19 [note: all are susceptible, throughout the age-range, and all are at cumulative risk of serious illness and death through reinfections], remains a paramount legal obligation.’
Professor Phil Banfield (BMA) & Dr. Barry Jones (CAPA) ~ (22 Dec 2023) ➲
❦ on shared air and swimsuits
“Coughing into one’s sleeve while in shared air is like peeing into one’s swimsuit while in shared water.”
Malgorzata Gasperowicz (2023)
❦ transmission ~ further reading
C-19 Archives:
transmission























❦ transmission: scientific papers & media articles
✒ 2023
📖 (15 Sep 2023 ~ CIDRAP/University of Minnesota) Study: Hospital wastewater system a 'highway' for resistant bacteria ➤
❂
📖 (8 Sep 2023 ~ Pre-print) Quantity of SARS-CoV-2 RNA copies exhaled per minute during natural breathing over the course of COVID-19 infection ➤
❂
📖 (8 Sep 2023 ~ Northwestern University) COVID patients breathe large amounts of virus early on ➤
➲ ‘COVID patients exhale high numbers of virus during the first eight days after symptoms start, as high as 1,000 copies per minute, reports a new Northwestern Medicine study.
On day eight, exhaled levels of virus drop steeply, down to near the limit of detection – an average of two copies exhaled per minute.’
❂
📖 (30 Aug 2023 ~ Nature: News) COVID infection risk rises the longer you are exposed – even for vaccinated people ➤
❂
📖 (19 Aug 2023 ~ Nature: Communications) Evidence of leaky protection following COVID-19 vaccination and SARS-CoV-2 infection in an incarcerated population ➤
❂
📖 (9 Aug 2023 ~ Pre-print) Long COVID in a highly vaccinated population infected during a SARS-CoV-2 Omicron wave – Australia, 2022 ➤
❂
📖 (2 Jun 2023 ~ CIDRAP/University of Minnesota) More than 70% of US household COVID spread started with a child, study suggests ➤
❂
📖 (21 Mar 2023 ~ World Health Network) Doctors Should Not Infect Patients ➤
❂
📖 (15 Mar 2023 ~ Journal of Clinical Medicine) Clinical Outcome and Prognosis of a Nosocomial Outbreak of COVID-19 ➤
❂
📖 (24 Feb 2023 ~ Journal of Hospital Infection) Impact of supplementary air filtration on aerosols and particulate matter in a UK hospital ward: a case study ➤
➲ ‘Collectively, this suggests that appropriately-sized air-cleaning units (ACUs) have the potential to reduce nosocomial infections, especially in inadequately ventilated hospital wards.’
❂
✒ 2022
📖 (16 Dec 2022 ~ JAMA Network Open: Infectious Diseases) Outbreak of SARS-CoV-2 Omicron Infection in a Centralized Quarantine Location in Hangzhou, China ➤
❂
📖 (27 Sept 2022 ~ Twitter) Jeff Gilchrist on Transmission ➤
❂
📖 (1 May 2022 ~ Open Forum Infectious Diseases) Initial Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load Is Associated With Disease Severity: A Retrospective Cohort Study ➤
➲ ‘Higher initial SARS-CoV-2 viral load is associated with an increased risk of hospital admission, ICU admission, and in-hospital mortality.’
❂
✒ 2021
📖 (27 Aug 2021 ~ Science) Airborne transmission of respiratory viruses ➤
➲ ‘There is robust evidence supporting the airborne transmission of many respiratory viruses, including measles virus, influenza virus, respiratory syncytial virus (RSV), human rhinovirus (hRV), adenovirus, enterovirus, severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2.
A growing body of research on COVID-19 provides abundant evidence for the predominance of airborne transmission of SARS-CoV-2. This route dominates under certain environmental conditions, particularly indoor environments that are poorly ventilated, an observation that implicates solely aerosols because only aerosols – and not large droplets or surfaces – are affected by ventilation.
Additional precautionary measures must be implemented for mitigating aerosol transmission at both short and long ranges, with a major focus on ventilation, airflows, air filtration, UV disinfection, and mask fit.
These interventions are critical strategies for helping end the current pandemic and preventing future outbreaks.’
❂
📖 (27 Aug 2021 ~ Science) Airborne transmission of respiratory viruses ➤
❂
📖 (13 May 2021 ~ Wired) The 60-Year-Old Scientific Screw-up That Helped Covid Kill ➤
‘All pandemic long, scientists brawled over how the virus spreads. Droplets! No, aerosols! At the heart of the fight was a teensy error with huge consequences.’
❂
📖 (4 May 2021 ~ Forbes) WHO Finally Admits Coronavirus Is Airborne. It's Too Late ➤
‘Over a year since declaring Covid-19 a pandemic, the World Health Organization has finally admitted that Coronavirus is airborne.’
❂
📖 (29 Mar 2021 ~ El País) Avoiding coronavirus infection in indoor spaces: don't breathe other people's air ➤
‘Constant ventilation and permanent control of CO₂ levels are two of the keys to avoiding transmission in closed rooms, as fresh air dilutes the infected particles.’
❂
📖 (25 Mar 2021 ~ Nature: Medicine) SARS-CoV-2 infection of the oral cavity and saliva ➤
❂
📖 (11 Mar 2021 ~ El País) Coronavirus: How infected air can flow from one apartment to another ➤
‘In Spain, the bathrooms of older buildings are connected through communal ducts that allow aerosol exchanges. Although not common, it is suspected that transmission may occur in specific circumstances.’
❂
✒ 2020
📖 (30 Oct 2020 ~ Science) The Science of Superspreading ➤
‘Why preventing hotspots of transmission is key to stopping the COVID-19 pandemic.’
❂
📖 (28 Oct 2020 ~ The Guardian) Understanding 'aerosol transmission' could be key to controlling coronavirus ➤
‘We should still wash our hands, but growing evidence suggests one of the main ways Covid-19 spreads is through the air.’
❂
📖 (25 Aug 2020 ~ Time) COVID-19 Is Transmitted Through Aerosols. We Have Enough Evidence, Now It Is Time to Act ➤
❂
📖 (20 Aug 2020 ~ The Conversation) Poor ventilation may be adding to nursing homes' COVID-19 risks ➤
‘Why are so many aged-care residents and staff becoming infected with COVID-19?
New research suggests poor ventilation may be one of the factors. RMIT researchers are finding levels of carbon dioxide in some nursing homes that are more than three times the recommended level, which points to poor ventilation.’
❂
📖 (25 Jun 2020 ~ Journal of Infection) Viral dynamics of SARS-CoV-2 in saliva from infected patients ➤
❂
📖 (17 Jun 2020 ~ The Conversation) I study coronavirus in a highly secured biosafety lab – here's why I feel safer here than in the world outside ➤
❂
📖 (27 May 2020 ~ Science) Reducing transmission of SARS-CoV-2 ➤
➲ ‘A large proportion of the spread of coronavirus disease 2019 (COVID-19) appears to be occurring through airborne transmission of aerosols produced by asymptomatic individuals during breathing and speaking.
Aerosols can accumulate, remain infectious in indoor air for hours, and be easily inhaled deep into the lungs.’
❂
📖 (14 Mar 2020 ~ Wired) They Say Coronavirus Isn't Airborne – But It's Definitely Borne By Air ➤
‘The word ‘airborne’ means different things to different scientists, and that confusion needs to be addressed.’
❂