on the body
On SARS-CoV-2 infections, reinfections, post-COVID-19 complications [Long Covid], and the human body.
Also see:
❦ on repeat infections
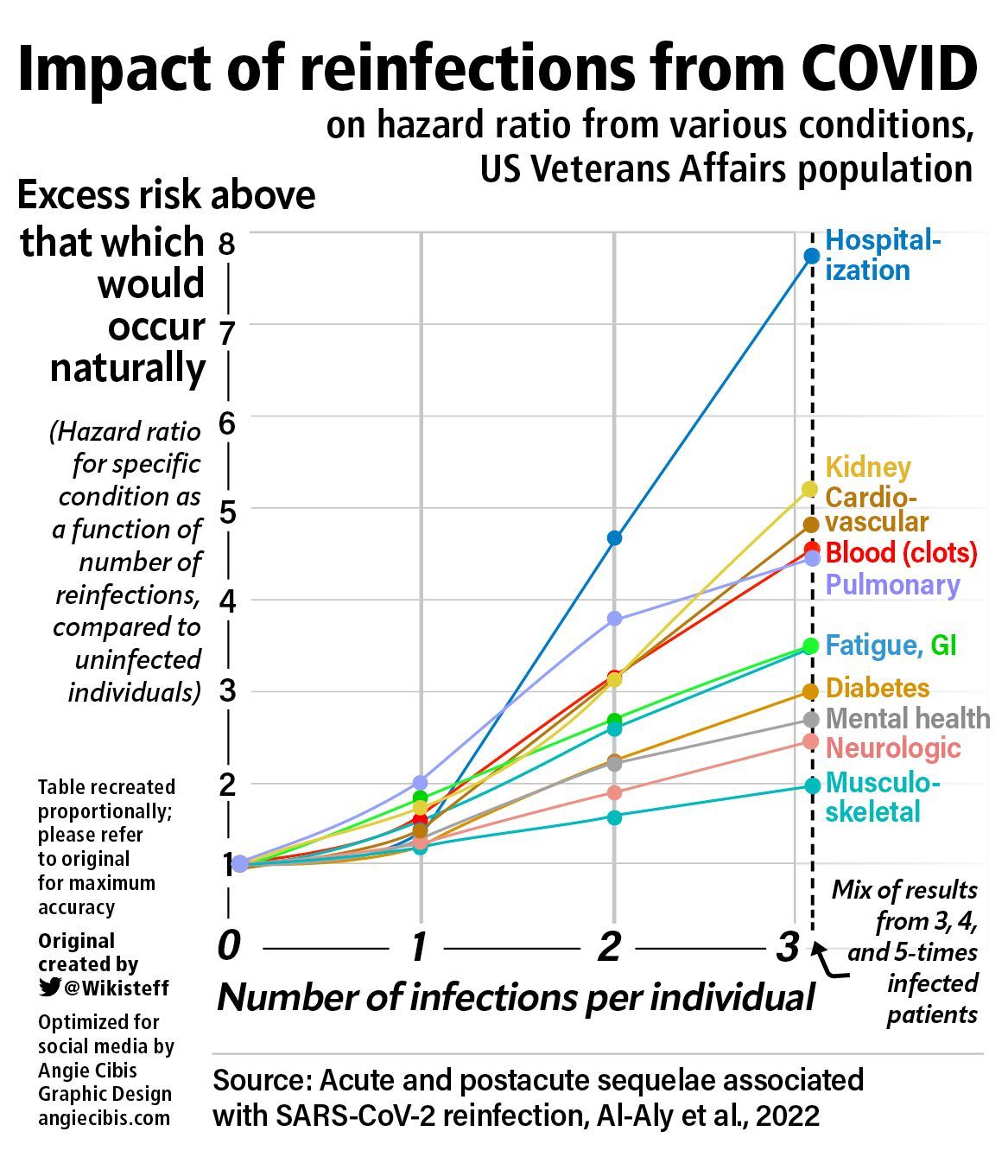
‘The data show a consistent pattern of increased likelihood of hospitalization, cardiovascular effects, clotting and other blood disorders, diabetes, fatigue, gastrointestinal distress, kidney damage, mental health effects such as depression, musculoskeletal damage, neurological deficits and pulmonary damage’ with each new reinfection.
‘The risk of hospitalization, organ damage and death rises markedly with repeat COVID-19 infection.’
Harvard Magazine (2022)
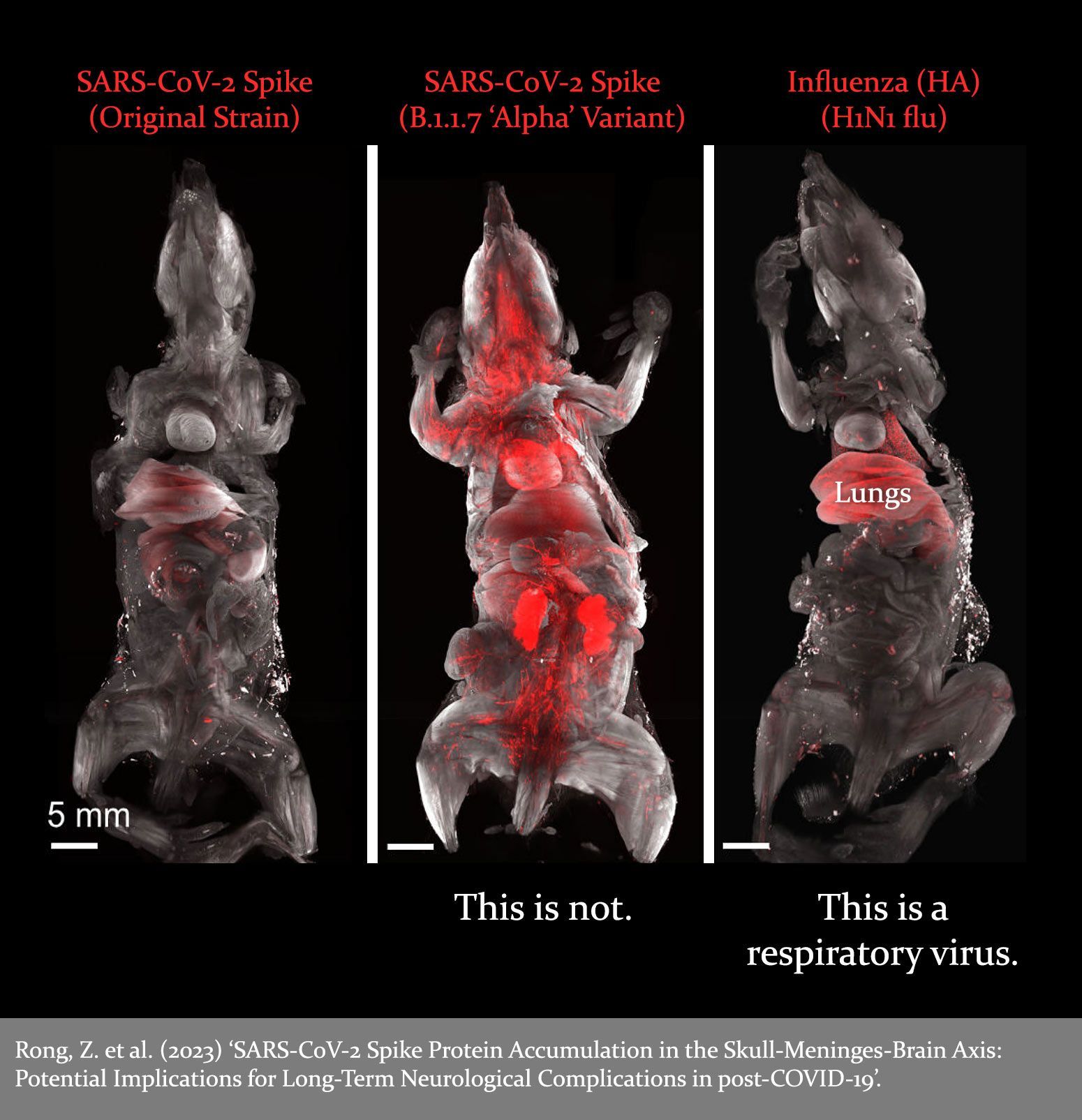
❦ on a mistaken early narrative
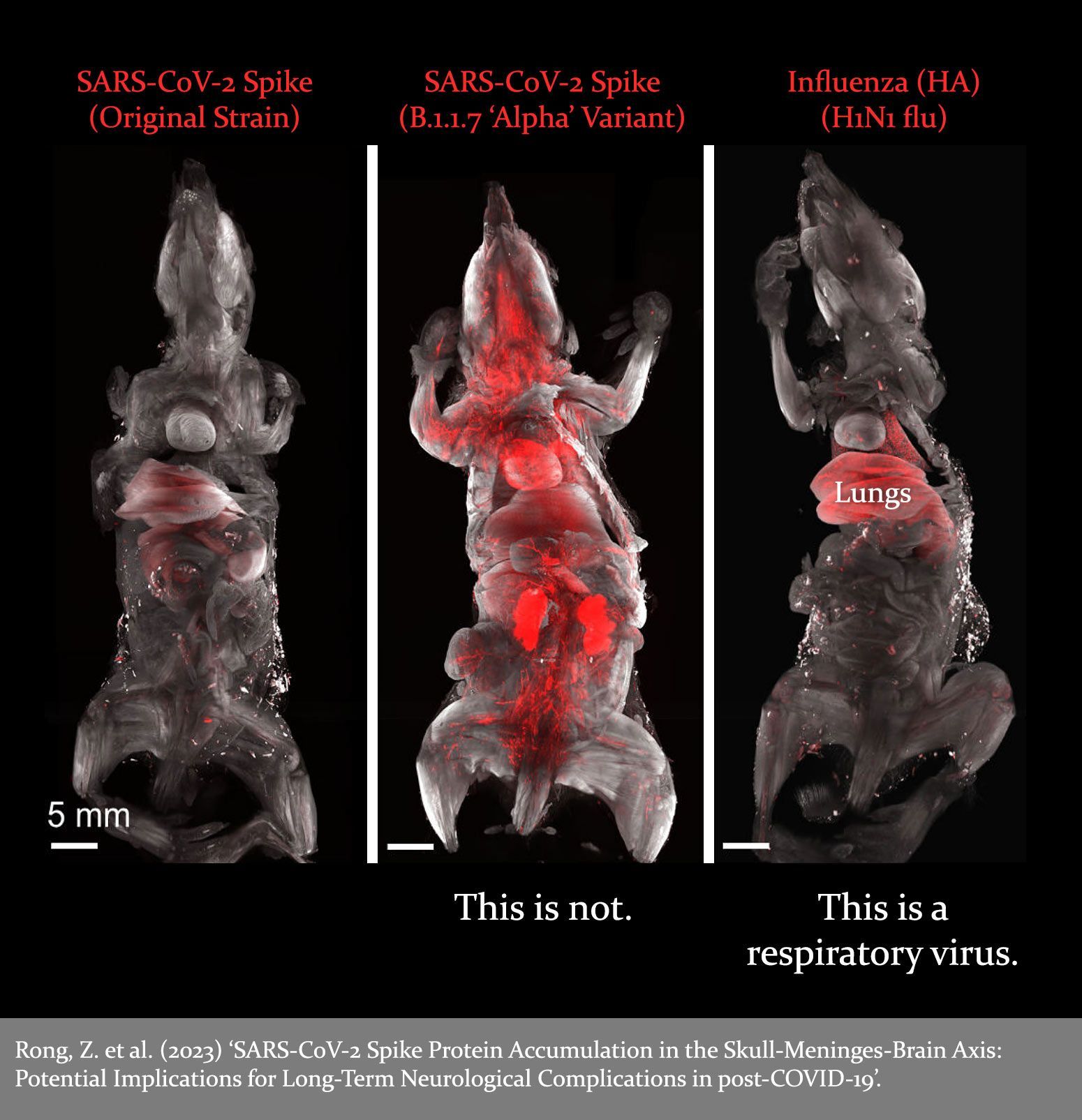
‘The narrative that COVID-19 had only respiratory sequelae led to a delayed realization of the neurological, cardiovascular and other multisystem impacts of COVID-19.’
❦ Sequelae = After-effect(s) of a disease, condition or injury.
❦ Neurological = A neurological disorder is any disorder of the nervous system.
❦ Cardiovascular = Relating to or involving the heart and blood vessels.
Davis et al (2023)
❦ A selection of potential acute / chronic complications following SARS-CoV-2 [COVID-19] infection(s).
❦ ‘Long COVID’ (LC) can affect anyone exposed to SARS-CoV-2 (the virus that causes COVID-19), regardless of age or severity of original symptoms.
Long COVID is also referred to as Post-COVID-19 Complications (PCC), Post-COVID-19 Syndrome (PCS), Post-COVID-19 Condition(s) (PCC), and Post-Acute Sequelae of COVID-19 (PASC).
It might be more simply understood as chronic COVID-19.
❂ Related:
❦ on unfathomable burdens, and forward planning
‘‘Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe.
The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new healthcare challenge.
The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia.
The oncoming burden of Long COVID faced by patients, healthcare providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it.’’
❦ Dysautonomia = A condition in which the autonomic nervous system (ANS) does not work properly. This may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels.
Professor Daniel M. Altmann et al (2023)
❦ on reinfections and post-COVID-19 complications
‘Getting reinfected worsens symptoms of Long COVID (post-COVID-19 complications), or triggers a recurrence of symptoms in people who have recovered.’
Australian Journal of General Practice (2021)
❦ on cancer, and trends
“The trend is getting more and more alarming.
We are noticing trends in hematological malignancies, breast cancer, colorectal carcinoma and pancreatic cancer.”
❦
Haematological malignancies
= Primary cancers of the blood and blood-forming organs, including bone marrow and lymphoid tissues.
Dr. Kashyap Patel (2023)
❦ on SARS-CoV-2, cancer onset, and accelerated cancer development
‘‘Recent research indicates that SARS-CoV-2 infection and COVID-19 progression may predispose recovered patients to cancer onset and accelerate cancer development.”
Costanzo et al (2023)
❦ on time-lag
‘SARS-CoV-2 can cause persistent infections in many parts of the body, months past an initial illness.
SARS-CoV-2 RNA was detected in
84 different locations
in the body. The
highest burden
of viral RNA
was found in
airway
and
lung tissue
– however, the virus was also detected in the
brain,
gut,
heart,
kidney,
eye,
adrenal gland
and
lymph nodes.’
Rich Haridy (2023)
❦ the body, reinfections & Long Covid ~ further reading














































C-19 Blog:
body












































❦ on erectile dysfunction (ED)
‘Statistics are significant regarding the link between COVID-19 and impotence.
“We found the risk of getting diagnosed with erectile dysfunction (ED) was about 20% higher in men who had COVID versus those who did not.”
Survey studies support the notion of a link between ejaculation difficulty and the virus – a study of nearly half a million adults published in Nature identified ejaculation difficulty and reduced libido as Long COVID symptoms in men.’
Carolyn Barber (2022)
❦ on risk
‘Death is not the main risk facing most children [with regard to SARS-CoV-2]. Disability is.’
Blake Murdoch (2023)
on babies and children
On SARS-CoV-2 infections and their effects on infants, babies, children and adolescents.
❦ one from 1958
‘To parody the words of Winston Churchill: never have so many been manipulated so much by so few.’
Aldous Huxley, ‘Brave New World Revisited’ (1958)
❦ on the body: scientific papers & media articles
✒ 2023
📖 (23 Sep 2023 ~ Time) Why You Should Rest – a Lot – If You Have COVID-19 ➤
❂
📖 (18 Sep 2023 ~ Diagnostics) Molecular Diagnosis of COVID-19 Sudden and Unexplained Deaths: The Insidious Face of the Pandemic ➤
❂
📖 (Accessed 17 Sep 2023 ~ US Govt/Covid.gov) What is Long COVID? Long COVID terms and definitions development explained ➤
❂
📖 (Accessed 16 Sep 2023 ~ RTHM) Viral Reactivation and Long COVID ➤
❂
📖 (Accessed 16 Sep 2023 ~ LCGAR: Long COVID Gene Association Resource) Long COVID – Phenotypes, Gene Association, Gene Ontology, Pathways and Drug repurposing ➤
❂
📖 (14 Sep 2023 ~ The John Snow Project) COVID-19: A New Disease Paradigm – What if SARS-CoV-2 continues to infect us even after the initial symptoms fade? ➤
❂
📖 (12 Sep 2023 ~ Genome Medicine) SARS-CoV-2 infection induces a long-lived pro-inflammatory transcriptional profile ➤
❂
📖 (4 Sep 2023 ~ The Lancet) Determinants of the onset and prognosis of the post-COVID-19 condition: a 2-year prospective observational cohort study ➤
❂
📖 (4 Sep 2023 ~ Nature: Immunology) SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC) ➤
❂
📖 (1 Sep 2023 ~ International Journal of Infectious Diseases) Presence of SARS-CoV-2 in middle ear fluid and characterization of otitis media with effusion in COVID-19 patients ➤
❂
📖 (9 Aug 2023 ~ Pre-print) Long COVID in a highly vaccinated population infected during a SARS-CoV-2 Omicron wave – Australia, 2022 ➤
❂
📖 (17 July 2023 ~ The Lancet) Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations ➤
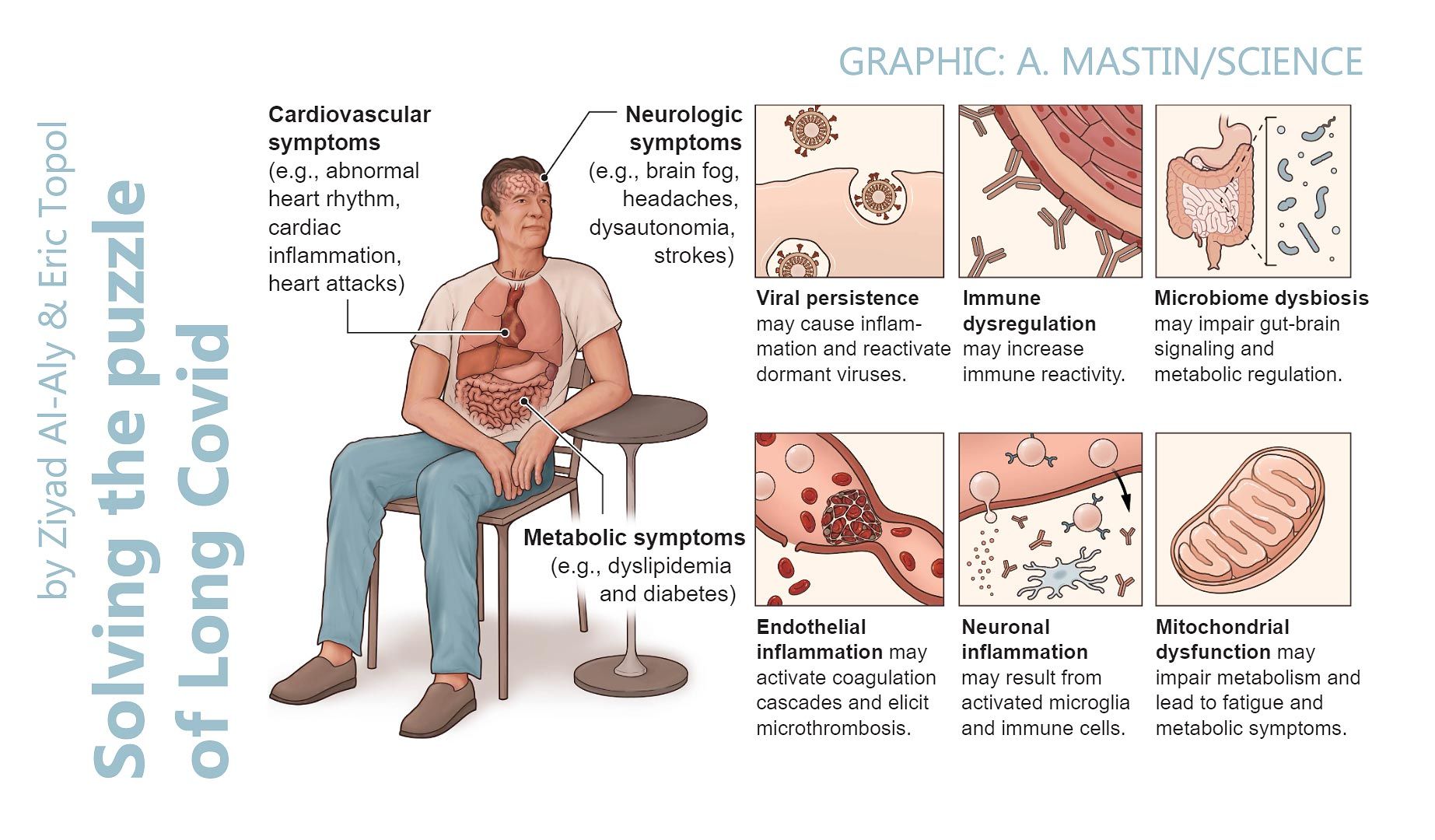
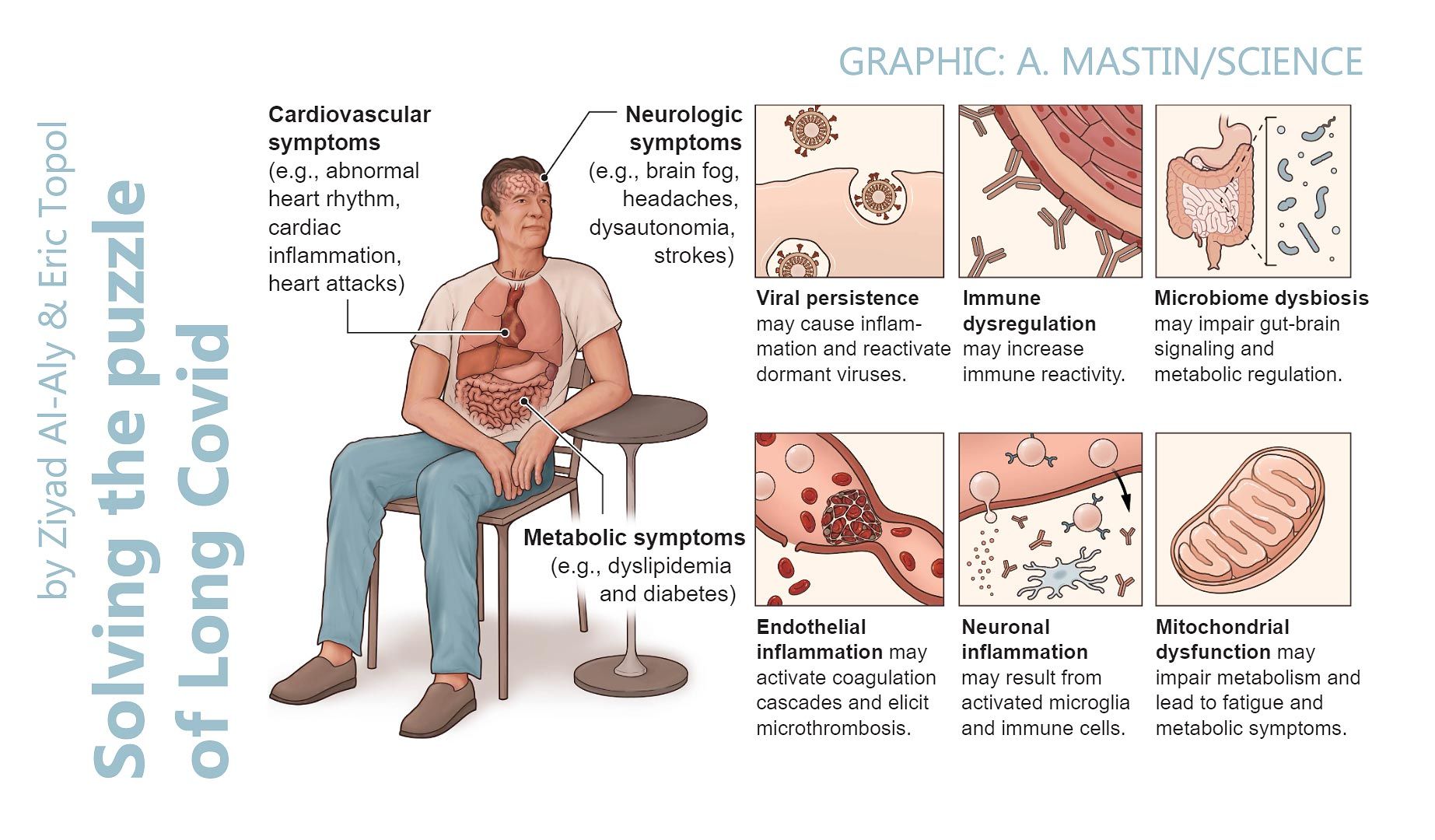
➲ 'Individuals with SARS-CoV-2 infection can develop symptoms that persist well beyond the acute phase of COVID-19 or emerge after the acute phase, lasting for weeks or months after the initial acute illness.
The post-acute sequelae of COVID-19, which include physical, cognitive, and mental health impairments, are known collectively as long COVID or post-COVID-19 condition (PCC).
The proportion of patients affected by post-COVID-19 condition might be in the range of 10–30% of those infected with SARS-CoV-2, although understanding of this condition is still evolving.
Socio-economic factors are fundamental determinants of health after COVID-19.
Individuals from low-income and middle-income countries, those from marginalised communities, and those who are socially disadvantaged are probably disproportionately affected.
The post-COVID-19 condition is systemic, affecting various organ systems.
PCC results in increased use of healthcare resources, a decreased quality of life, an increased susceptibility to subsequent viral or bacterial infection, and leads to heightened vulnerability to perioperative morbidity and mortality for individuals who require a surgical procedure for any (unrelated) indication.
With a large and growing global population of survivors of COVID-19, the impact on individuals, healthcare systems, communities, and society is likely to be substantial.
At present, there are no specific treatments for post-COVID-19-condition.'
❂
📖 (11 July 2023 ~ Nature Reviews: Immunology) The immunology of long COVID ➤
➲ 'Long COVID is the patient-coined term for the disease entity whereby persistent symptoms ensue in a significant proportion of those who have had COVID-19, whether asymptomatic, mild or severe.
The disease burden spans from mild symptoms to profound disability, the scale making this a huge, new healthcare challenge.
Long COVID will likely be stratified into several more or less discrete entities with potentially distinct pathogenic pathways.
The evolving symptom list is extensive, multi-organ, multisystem and relapsing–remitting, including fatigue, breathlessness, neurocognitive effects and dysautonomia.
A range of radiological abnormalities in the olfactory bulb, brain, heart, lung and other sites have been observed in individuals with Long COVID.
Some body sites indicate the presence of microclots; these and other blood markers of hypercoagulation implicate a likely role of endothelial activation and clotting abnormalities.
Diverse auto-antibody (AAB) specificities have been found, as yet without a clear consensus or correlation with symptom clusters.
There is support for a role of persistent SARS-CoV-2 reservoirs and/or an effect of Epstein-Barr virus reactivation, and evidence from immune subset changes for broad immune perturbation.
The oncoming burden of Long COVID faced by patients, healthcare providers, governments and economies is so large as to be unfathomable, which is possibly why minimal high-level planning is currently allocated to it.'
❂
📖 (5 Jun 2023 ~ CIDRAP/University of Minnesota) Study finds 27% rate of long COVID in infected health workers ➤
❂
📖 (23 May 2023 ~ Biochimie) Possible cancer-causing capacity of COVID-19: Is SARS-CoV-2 an oncogenic agent? ➤
❂
📖 (17 May 2023 ~ News Medical) Post-COVID condition varies by variant and vaccination status ➤
❂
📖 (10 May 2023 ~ The Lancet) Association of SARS-CoV-2 infection and persistence with long COVID ➤
➲ 'Long COVID or post-COVID-19 condition (PCC) can affect anyone exposed to SARS-CoV-2, regardless of age or severity of the original symptoms, characterised by long-term health problems persisting or appearing after the typical recovery period of COVID-19.
The presented evidence suggests that the duration of SARS-CoV-2 infection in patients can persist considerably longer than suggested by PCR-negative tests on nasopharyngeal swabs or bronchoalveolar lavage fluids.
A US study including 40,947 participants with SARS-CoV-2 reinfection (two or more infections) indicated that reinfection further increases risks of death, hospitalisation, and sequelae in multiple organ systems in the acute and post-acute phases.'
❂
📖 (25 Apr 2023 ~ International Journal of Molecular Sciences) Deciphering the Relationship between SARS-CoV-2 and Cancer ➤
➲ 'Some viruses are known to be associated with the onset of specific cancers.
These micro-organisms – oncogenic viruses or oncoviruses – can convert normal cells into cancer cells.
Seven oncogenic viruses are known to promote tumorigenesis [tumour creation] in humans: human papillomavirus (HPV), hepatitis B and C viruses (HBV, HCV), Epstein-Barr virus (EBV), human T-cell leukemia virus 1 (HTLV-1), Kaposi sarcoma-associated herpesvirus (KSHV), and Merkel cell polyomavirus (MCPyV).
Recent research indicates that SARS-CoV-2 infection and COVID-19 progression may predispose recovered patients to cancer onset and accelerate cancer development.
This hypothesis is based on the growing evidence regarding the ability of SARS-CoV-2 to modulate oncogenic pathways, promoting chronic low-grade inflammation and causing tissue damage.'
❂
📖 (24 Apr 2023 ~ European Archives of Oto-Rhino-Laryngology) Hearing loss and COVID-19: an umbrella review ➤
❂
📖 (22 Mar 2023 ~ Evidence-Based Oncology) Kashyap Patel, MD, Sees Link Between COVID-19 and Cancer Progression, Calls for More Biomarker Testing ➤
➲ 'Kashyap Patel, MD, CEO of Carolina Blood & Cancer Care Associates, sees something different in his practice since the onset of the COVID-19 pandemic – not just with cancer care, but with cancer itself.
“The trend is getting more and more alarming. We are noticing trends in hematological malignancies, breast cancer, colorectal carcinoma and pancreatic cancer.”
With COVID-19 added to the mix, Patel now fears a “perfect storm” of factors will trigger inflammatory responses in some patients, causing cancer to arrive years earlier than normal and making it deadlier once it is diagnosed.'
❂
📖 (1 Mar 2023 ~ Scientific American) Long COVID Now Looks like a Neurological Disease, Helping Doctors to Focus Treatments ➤
❂
📖 (27 Feb 2023 ~ eClinicalMedicine/The Lancet) Multiomic characterisation of the long-term sequelae of SARS survivors: a clinical observational study ➤
❂
📖 (23 Feb 2023 ~ News Medical Life Sciences) Pathogenicity of SARS-CoV-2 viral components on human periodontal tissues and cells ➤
❂
📖 (22 Feb 2023 ~ Journal of Orthopaedic Research) Acute bone loss following SARS-CoV-2 infection in mice ➤
❂
📖 (16 Feb 2023 ~ Nature Medicine) Comorbidities, multimorbidity and COVID-19 ➤
❂
📖 (20 Jan 2023 ~ International Journal of Molecular Medicine) Digestive system infection by SARS‑CoV‑2: Entry mechanism, clinical symptoms and expression of major receptors (Review) ➤
❂
📖 (18 Jan 2023 ~ Pathological Society) Persistent SARS-CoV-2 infection in patients seemingly recovered from COVID-19 ➤
❂
📖 (13 Jan 2023 ~ Nature Reviews / Microbiology) Long COVID: major findings, mechanisms and recommendations ➤
➲ 'Long COVID is a multi-systemic illness encompassing ME/CFS, dysautonomia, impacts on multiple organ systems, and vascular and clotting abnormalities.
It has already debilitated millions of individuals worldwide, and that number is continuing to grow.
On the basis of more than 2 years of research on Long COVID and decades of research on conditions such as ME/CFS, a significant proportion of individuals with Long COVID may have lifelong disabilities if no action is taken.
Diagnostic and treatment options are currently insufficient, and many clinical trials are urgently needed to rigorously test treatments that address hypothesized underlying biological mechanisms, including viral persistence, neuroinflammation, excessive blood clotting and autoimmunity.'
❂
📖 (9 Jan 2023 ~ Science Alert) COVID Autopsies Reveal The Virus Spreading Through The 'Entire Body' ➤
❂
✒ 2022
📖 (14 Dec 2022 ~ Nature) SARS-CoV-2 infection and persistence in the human body and brain at autopsy ➤
➲ 'Others have previously reported SARS-CoV-2 RNA within the heart, lymph node, small intestine and adrenal gland.
We replicate these findings… and we conclusively demonstrate that SARS-CoV-2 is capable of infecting and replicating within... the heart, lymph node, small intestine, adrenal gland... respiratory tissues... and brain.
The virus can disseminate throughout the entire body.’
❂
📖 (22 Nov 2022 ~ National Institutes of Health/NIH) COVID-19 disrupts gut microbiome ➤
❂
📖 (28 Sep 2022 ~ The Tyee) The Coming COVID Brain Wreck? ➤
➲ 'A new study adds to concerns about the severity and scope of neurological damage the virus can cause.'
❂
📖 (23 Sep 2022 ~ CTV News/Canada) COVID raises risk of long-term brain injury, large U.S. study finds ➤
❂
📖 (22 Sep 2022 ~ Nature: Medicine) Long-term neurologic outcomes of COVID-19 ➤
❂
📖 (9 Aug 2022 ~ Journal of Infection) Is SARS-CoV-2 an oncogenic virus? ➤
❂
📖 (28 Apr 2022 ~ The Lancet) Long-term mortality following SARS-CoV-2 infection: A national cohort study from Estonia ➤
❂
✒ 2021
📖 (18 Nov 2021 ~ Forbes) Covid Ear: Virus Implicated ➤
❂
📖 (26 Aug 2021 ~ Journal of Oral Microbiology) Mycotic infections – mucormycosis and oral candidiasis associated with Covid-19: a significant and challenging association ➤
❂
📖 (7 Jun 2021 ~ International Journal of Molecular Science) Evidence for Biological Age Acceleration and Telomere Shortening in COVID-19 Survivors ➤
❂
📖 (23 Mar 2021 ~ Annals of Clinical and Translational Neurology) Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 "long haulers" ➤
❂
📖 (16 Feb 2021 ~ Neurogastroenterology & Motility) Implications of SARS‐CoV‐2 infection for neurogastroenterology ➤
❂
📖 (1 Jan 2021 ~ International Journal of Biological Sciences) A Multiple-Hit Hypothesis Involving Reactive Oxygen Species and Myeloperoxidase Explains Clinical Deterioration and Fatality in COVID-19 ➤
➲ 'Multi-system involvement is a hallmark of COVID-19.
Although direct viral spread to distant organs is a possibility, release of inflammatory mediators and downstream messengers are also likely important effectors of physiological systems.
Major physiological systems affected in COVID-19 include, primarily, the respiratory and cardiovascular system, as well as the renal, hepatic, and nervous systems.'
❂
✒ 2020
📖 (5 Aug 2020 ~ Frontiers in Medicine) Single Virus Targeting Multiple Organs: What We Know and Where We Are Heading? ➤
➲ 'The common symptoms of [COVID-19] include dry cough, fatigue, and fever. Sore throat, nasal congestion, body aches, and pains are also common.
However, several other manifestations related to the heart, lungs, liver, kidney, central nervous system, and gastrointestinal system failure is making treatment difficult for critically ill patients.
The presence of ACE2 receptors throughout the human body provides an opportunity for the virus to invade different organs easily and is a possible explanation why multiple-organ damage has been reported in many patients.'
❂
📖 (15 Jul 2020 ~ The Journal of Bone & Joint Surgery) Musculoskeletal Consequences of COVID-19 ➤
❂
📖 (24 Apr 2020 ~ Science) A rampage through the body ➤
➲ 'The lungs are ground zero, but COVID-19 also tears through organ systems from brain to blood vessels.
Clinicians and pathologists are struggling to understand the damage wrought by the coronavirus as it tears through the body.
They are realizing that although the lungs are ground zero, the virus' reach can extend to many organs including the heart and blood vessels, kidneys, gut, and brain.
“COVID-19 can attack almost anything in the body with devastating consequences,” says cardiologist Harlan Krumholz of Yale University and Yale-New Haven Hospital, who is leading multiple efforts to gather clinical data on COVID-19.
“Its ferocity is breathtaking and humbling.”
❂
❦ postscript
You are free to disagree with anything you read here, provided that you have an authentic, evidence-based argument for it.
❦ All content on this website is for informational and educational purposes only.
c19.life